Which Covid-19 drugs work best?
Results are in from the first organized trials of drugs to treat Covid-19, but so far, there’s no cure.
As the new respiratory disease spread widely starting in January, doctors—first in China and then in the US, Italy, and France—all moved to test readily available drugs that are used for other purposes and are fairly safe. Now, just three months into the pandemic, the first medical results from organized trials—studies structured to measure whether a drug actually helps—are becoming public. We count three so far, all involving drugs with antiviral properties.
Patients who end up in the ICU are begging for whatever treatment they can get, and demand for drugs will skyrocket in the US. Not only is the number of confirmed cases now over 35,000, but this week twice that many or more will likely feel the onset of typical symptoms like cough, fever, and shortness of breath.
You can read all our coverage of the coronavirus/Covid-19 outbreak for free, and also sign up for our coronavirus newsletter. But please consider subscribing to support our nonprofit journalism.
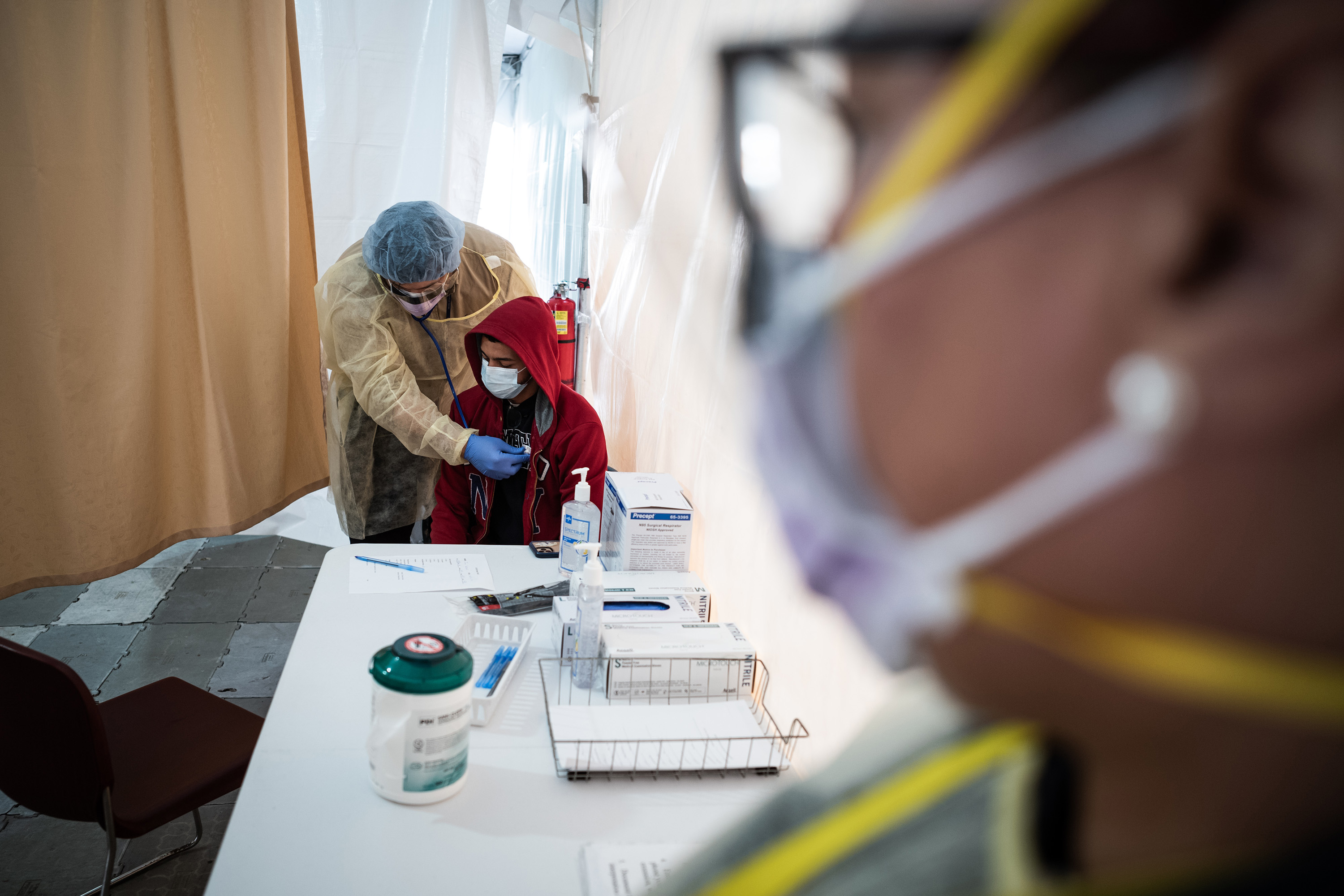
So far, there is no approved medicine for Covid-19, so the main treatment for severe cases isn’t drugs at all—it’s oxygen therapy, ventilators that help people breathe, and supportive care. Some patients get standard antibiotics.
Overall, scores of drug studies are under way, checking the benefits of everything from vitamin C to Chinese traditional medicine. A list of trials compiled by CellTrials.org, a consultancy, found that doctors had registered over 250 Covid-19 studies, mostly in China, and were seeking to recruit 26,000 patients. It may be another month before some other large, important studies, like several involving the experimental antiviral remdesivir, made by the US company Gilead, are ready to report any findings.
Here are the facts about the drug studies published so far.
Chloroquine or hydroxychloroquine
The hype: President Donald Trump praised the malaria drug, saying it had shown “tremendous promise” against Covid-19. “I think it’s going to be very exciting,” he said. “I think it could be a game-changer, and maybe not.”
The data: During early March, French doctors at IHU-Méditerranée Infection in Marseille, France, treated Covid-19 patients with hydroxychloroquine, a version of the 90-year-old malaria drug chloroquine. They tried giving 200 milligrams of hydroxychloroquine three times per day, over 10 days, to 26 patients, and some got the antibiotic azithromycin, too. In their report, treated patients had less virus in their system after six days than other patients at a different center, who didn’t get the treatment. The study’s conclusions aren’t firm because so few patients were involved and the study was not rigorously designed, although chloroquine has also been tried in China with rumors of success.
So does the drug work? Scientists say there’s not enough evidence to say. “Anecdotal reports may be true, but they are anecdotal,” Anthony Fauci, head of the National Institute of Allergy and Infectious Diseases, said during a briefing at the White House. “It was not done in a controlled clinical trial. So you really can’t make any definitive statement about it.”
In the absence of other options, Governor Andrew Cuomo of New York said his state, now a global epicenter of Covid-19, had obtained 70,000 doses of hydroxychloroquine and 750,000 doses of chloroquine, as well as azithromycin (also called Zithromax). “The trial will start this Tuesday,” said Cuomo over the weekend. “There is a good basis to believe they could work. The president ordered the FDA to move and the FDA moved.”
Chloroquine has risks, because it can affect heart rhythm. No one should take it without a prescription.
Favipiravir
The hype: News reports last week claimed Chinese officials had touted this antiviral medicine made in Japan as “clearly effective.”

The report: Favipiravir versus Arbidol for COVID-19: A Randomized Clinical
Trial
The data: While favipiravir, an antiviral made by Toyama Chemical (part of Fuji Film), generated hopeful headlines, the report from doctors at China’s Wuhan University makes more modest claims. They organized a study of 240 “ordinary” patients (meaning they had pneumonia but were not the worst cases) around Hubei province. Half got favipiravir and half got umifenovir (or Arbidol), an antiviral used in Russia, and they were watched to see which group recovered faster. The doctors found that patients’ fevers and coughs went away faster on favipiravir, but similar numbers in each group ended up needing oxygen or a ventilator. On the basis of these findings, they concluded that favipiravir is the “preferred” of the two drugs.
Favipiravir, which is known by the trade name Avigan in Japan, inhibits viruses from copying their genetic material. It was originally discovered while searching for drugs to treat influenza.
Lopinavir and ritonavir
The hype: Doctors reached into the cabinet of advanced anti-HIV medications, hoping for a quick success.

The report: A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19
The data: This is the largest, best-organized study of a treatment for Covid-19 so far, but it didn’t find a benefit. In January, doctors in China randomly assigned 199 patients with pneumonia either to get the HIV medicines lopinavir and ritonavir twice a day for two weeks, or to receive only standard care. Then they watched to see who improved or got discharged from the hospital. Unfortunately, no benefit was seen from the treatment. Nearly 20% of the patients died. The team wonders if the drug combo, sold in the US by AbbVie to treat HIV infection under the trade name Kaletra, could still prove beneficial for less sick patients.
The key drug here is lopinavir, a protease inhibitor, which has been shown in lab and animal tests to have effects against Middle East respiratory syndrome coronavirus, or MERS. Ritonavir acts to increase the first drug’s availability in the body.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.