One woman’s race to defuse the genetic time bomb in her genes
In 2011, Sonia Vallabh was handed a genetic report that contained a death sentence. But it also held a map for how to escape.
Her body, she learned, harbored a gene mutation, a single wrong letter of DNA in her “prion” gene, that would eventually lead to a rare brain condition called fatal familial insomnia. Her mother had died of it the year before, and the test had revealed Vallabh had inherited the flaw too.
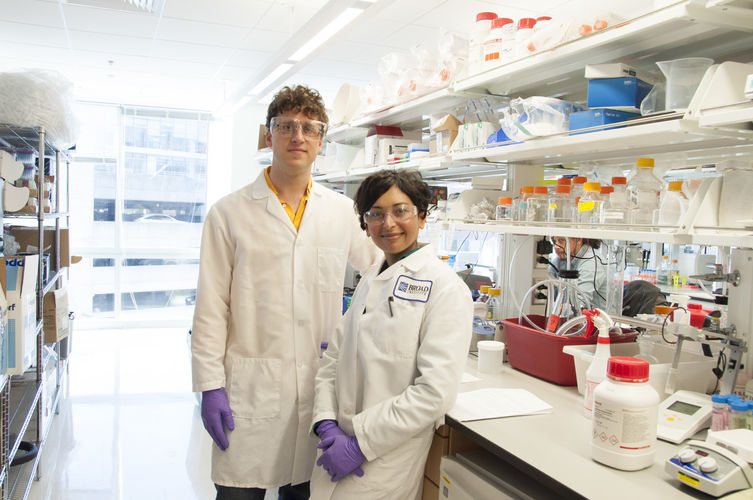
By now, the decision by Vallabh and her husband, Eric Minikel, to try to prevent her disease—“a prion love story,” the New Yorker called it—is well-known. After the diagnosis of the genetic time bomb, they dropped out of their careers in law and engineering and became scientists dedicated to defusing it. They expect to get PhDs next spring (see “Sonia Vallabh, 35 Innovators Under 35, 2016”.)
Now, after seven years, they think they have found a treatment that can do it. It’s called an antisense drug, a type of mirror-image molecule that, if it reaches the brain, could greatly reduce the amount of the prion protein. That could potentially forestall the mysterious chain reaction of misfolding proteins that characterize prion diseases.
Less of the protein, Vallabh reasons, and less chance she’ll get sick.
Two weeks ago, on their blog, Vallabh announced she and Minikel were working with a commercial partner, the California biotech company Ionis, which specializes in antisense compounds. “For the first time, I am optimistic about a specific therapeutic strategy,” she wrote. It’s “plausible” that antisense could treat the disease “in our lifetime.”
Vallabh’s race to prevent her own prion disease raises a question for the genetic age. Given a perfect DNA blueprint of your inherited disease, what’s your chance of stopping it in your lifetime, or that of someone you love?
There are reasons to think these types of medical long shots have become more likely to hit the mark. That is because gene sequencing can cheaply reveal molecular flaws, but also because a set of promising technologies—antisense, gene therapy, and CRISPR gene editing—are able to replace genes or silence them, in effect fixing genetic problems at their source.
What’s more, these treatments employ the genetic code; they are actually made of DNA or RNA. That means that they’re fundamentally modular and programmable. At least on paper, it is now possible to take any genetic flaw and quickly sketch an antidote.
In reality, drug development is notoriously complicated. Most drugs fail, torn down by biological surprises and unexpected toxicity to the human body. But Vallabh says in the early, confusing days of her quest, she received critical advice from Eric Lander, the biologist who leads the Broad Institute, where she and Minikel now study and work. He told her to focus on the genetic error itself—the blueprint of which was in her diagnosis.
“You need to see what you have in your hand and stop looking,” she recalls him saying.
That meant not waiting to answer important scientific unknowns, like what the prion protein does in the body, or why, when it misfolds, it kills brain cells. “There are so many interesting questions about prion disease,” says Vallabh, who is 34. “And those questions will still be there when we are treating it.”
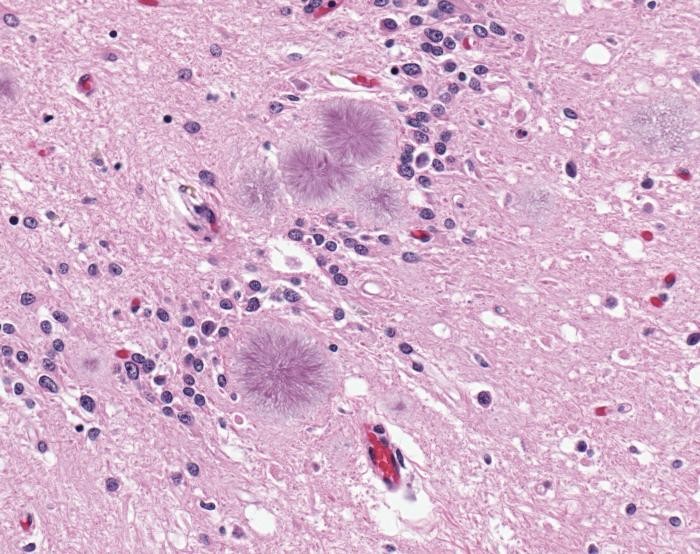
Prion diseases are profoundly strange because they’re caused not by a virus, but by an infectious protein. They include scrapie in sheep, Kuru (spread by cannibalism), Creutzfelt-Jakob disease, and the human version of mad cow disease.
The key drug insight was that mice engineered to lack the prion protein gene never get sick, even when scientists inject infectious prions into their brains. “The biological concept of a prion is a protein that changes it conformation, and that can template further copies. It’s self-templating. That allows it to spread,” says Kurt Giles, a researcher in the lab at the University of California, San Francisco, where prions were first discovered. “That leads to the idea of reducing the [protein]. The less of it there is, then you will get less templating.”
For genetic therapies, though, there’s a further problem, which is how to get them into the body so that they reach, for instance, billions of brain cells.
Antisense technology, conceived decades ago, had its big breakthrough last year when a drug developed by Ionis proved to be astoundingly effective in treating a childhood neurological disorder, spinal muscular atrophy.
By then, Vallabh and Minikel had been introduced to Ionis, and the company had agreed to provide them with antisense compounds targeted to the prion gene to test in mice. Holly Kordasiewicz, the head of neuroscience at Ionis, recalls the 2014 meeting. “We left the room saying we need to do everything that we can to help these people,” she says.
The company gave Vallabh and Minikel a to-do list, which they quickly worked through. Patient registry? Check. Animal studies? Check. Biomarker to show if a drug is working? That research, too, is under way at a Boston hospital studying prion protein levels in spinal fluid.
“Sonia and Eric are doing this with no real funding, just trying to make it happen,” says Jeff Carroll, another patient scientist (he’s got the mutation for Huntington’s disease), who introduced them to Ionis.
One problem not as easily addressed is that prion disease is astoundingly rare, quickly fatal, and rarely diagnosed in advance. That means there has been no great clamor for treatments. Maybe only 200 people in the U.S. know they have a time bomb like Vallabh, she says, and there’s not a single drug currently in human testing. Early on, Ionis let the pair know the collaboration was strictly academic and not a commercial prospect.
But by blotting out the prion protein at its source, an antisense treatment might help with a range of rare conditions linked to it. Fatal insomnia is vanishingly uncommon, as are cases of mad cow disease, but adding these “ultra-rare” diseases together makes them, as a group, slightly less rare.
Vallabh and Minikel say they now have proof that Ionis’s antisense molecules partly protect mice from prion disease. Those animals given the drug live about 70 percent longer.
Kordasiewicz now terms the program a “commercial” project at Ionis, though it remains too small and early-stage to appear on the company’s pipeline chart of drugs under development. “What changed is the data is looking good enough that we think we can have a drug in five years,” she says.
Vallabh hopes it can all go even faster. The fatal insomnia could begin to afflict her tomorrow, or in 30 years. There’s no way to predict it. She and Minikel just had their first child. The girl was conceived through IVF, and Vallabh says the lab employed a genetic test to assure them she wouldn’t carry the mutation.
To save herself, it’s not going to be enough to have a drug. She needs to get it before she ever falls ill. Yet doctors have little experience giving such a genetic drug over many years as a form of prevention.
Figuring out how to carry off such a study is the next challenge for Vallabh and her husband. It appears they hope the US Food and Drug Administration will permit a prevention trial in patients who carry the prion mutations. Since it can take decades for people to get sick (or not), such a study would instead rely on a biomarker, such as whether antisense injections can reduce prion protein levels in the spinal fluid.
Vallabh told me she would volunteer to take the drug. “The big picture,” she says, “is we are moving much more quickly than anyone could expect due to this beautifully clear genetic blueprint we were handed.”
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
Google helped make an exquisitely detailed map of a tiny piece of the human brain
A small brain sample was sliced into 5,000 pieces, and machine learning helped stitch it back together.
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.