Will Embryonic Stem Cells Ever Cure Anything?

When his son Sam was diagnosed with type 1 diabetes at six months of age, Doug Melton was incredulous. “I remember at night, my wife and I pricking his heel, and saying ‘No, this can’t be, this can’t be,’” he says. “It felt like we had lost the lottery.”
Later, his daughter would receive the same diagnosis. By then, Melton had already dropped what he was doing—studying frog eggs at Harvard—and launched an effort to grow pancreatic cells from scratch in his lab. The beta cells of the pancreas are the ones killed off in type 1 diabetes, and Melton reasoned he could replace them using new tissue manufactured from embryonic stem cells.
Melton’s effort, involving a 30-person lab at Harvard and a startup company, Semma Therapeutics, which he named after his children, Sam and Emma, is one of the most costly and sustained efforts to turn stem cells into transplantable tissue, an attempt that Melton admits has been full of false starts and dead ends. “The public definitely doesn’t appreciate that much of science is failure,” he says.
In fact, no field of biotechnology has promised more and delivered less in the way of treatments than embryonic stem cells. Only a handful of human studies has ever been carried out, without significant results. The cells, culled from IVF embryos, are capable of developing into any other tissue type in the body, and therefore promise an unlimited supply of replacement tissue.
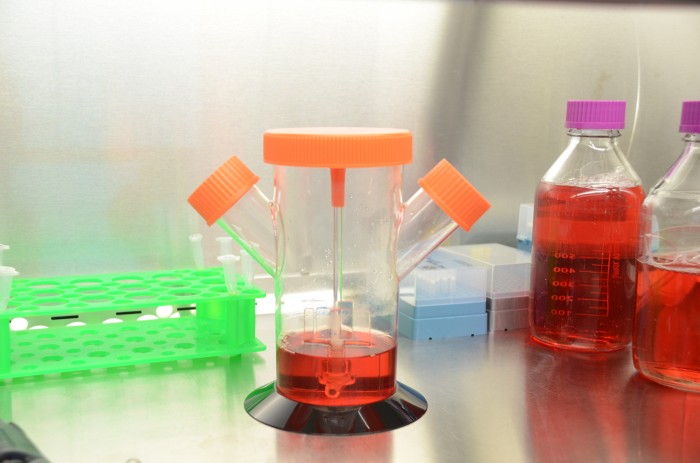
Sounds simple, but it hasn’t been. It took Melton and his team 15 years to unveil each molecular step required to coax a stem cell into a pancreatic beta cell able to sense glucose and secrete insulin. The recipe uses a cocktail of chemicals and a three-dimensional incubation system, tall spinning flasks brewing what looks like murky red Gatorade, that within 30 days can direct the differentiation of stem cells into fully functional beta cells.
Earlier this year, Melton was finally able to demonstrate he could control blood glucose levels of mice for six months using transplants of human beta cells. He thinks he can do that in humans and stretch the therapeutic effect out to a year, a goal that’s been turned over to Semma, which is designing an implantable pouch to hold and protect the cells.

Over the last two years, Semma has raised just under $50 million from venture capital firms, California's stem-cell agency, and corporate partners including Novartis and Medtronic. William Sahlman, a Harvard Business School professor who sits on Semma's board, says “people are prepared to put very large amounts of money on the experiments.” One reason: the global market for insulin exceeds $30 billion a year. Tests strips and monitors might double that.
Because their bodies mount an immune attack on the pancreatic cells that regulate blood glucose, type 1 diabetics are constantly measuring their blood sugar levels with finger pricks and injecting insulin multiple times a day. Their lives can be foreshortened by more than a decade. “You could almost say that cellular therapy is the natural solution,” Melton says. “It’s not the technological solution. It’s not the Google solution. It’s nature’s solution to the problem. You’re providing the cell which is missing.”
Several companies are attempting a tech solution, however, by using electronics to build an artificial pancreas that combines a continuous glucose monitor, an insulin pump, and a sensor with an algorithm to control dosing. Medtronic is nearing FDA approval with one such “closed loop” system; its smartphone-sized MiniMed 670G performed well in early trials. One of Google’s sister companies, Verily, is itself developing glucose-sensing contact lenses and ultra-thin sensors.
San Diego-based ViaCyte, working with Johnson & Johnson, was first to try pancreatic cells derived from embryos in people. It has built an implantable packet of immature cells, which it hopes will differentiate inside the body, and last year opened a clinical trial to test the idea.
Semma also thinks it needs to turn embryonic stem cells into not only insulin-secreting beta cells, but a full-fledged islet—the cluster of cells that includes the alpha, beta, delta, and ancillary cells normally found in a pancreas. That’s a complex objective but one that closely mimics biology. “There’s a reason during evolution that these cells are adjacent to one another,” says Felicia Pagliuca, Semma's cofounder and a veteran of Melton’s lab.
In order to deliver their lab-grown islet to diabetics, Semma is developing prototypes of an iPhone-sized, retrievable packet whose materials insulate it from the immune system, so that patients don’t have to take immune-suppressing drugs, as they would if they had a kidney transplant. Christopher Thanos, Semma's vice president of delivery, says his team is modeling physiological processes inside and around the device to experiment with different rates of oxygen, nutrients, and insulin diffusion.
Some outside experts think protecting the cells will not be possible. “I'm not optimistic that encapsulation is going to provide the answer,” says David Cooper, a professor of surgery at the University of Pittsburgh working on growing human islets in pigs. “I personally don't think a device is ever going to be successful. It's impossible to keep all the injurious agents out,” he says, referring to the cytokines, antibodies, and other compounds the body releases in response to a foreign body. “There's really very little evidence that a capsule can protect you completely from an immune response.”
The prospect of surgery every year for the rest of your life is also a practical concern. How many diabetics would sign up for 50, 60, 70 surgeries over the course of a lifetime? What will be the effect of repeated scarring around the surgical site? Melton says the inconvenience of surgery has to be weighed against the thousands of finger pricks and injections that diabetics must administer every year. “My kids say once a month they wouldn’t hesitate. I think that’s a bit extreme,” he says. “But if it was twice a year, I think that’s a go.”
If the device does not work, Semma has a backup plan of sorts. It received a $5 million grant from CIRM, the California stem-cell agency, to manufacture islets out of a patient's own tissue using induced pluripotent stem cells. That is a process by which adult cells, like skin cells, are reprogrammed into stem cells. Such matching cells wouldn’t be rejected by the body as foreign—and might not need as much protection—although they probably would not avoid damage by the processes that cause type 1 diabetes in the first place. Semma believes they could help a fraction of patients whose diabetes has different causes.
Semma still has no timeline for when its implantable biotech pancreas could be ready. That means Melton's children will have to wait a while longer. “I’m sorry it takes so long,” says Melton, “but it is going to work.”
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.