The Painkillers That Could End the Opioid Crisis
It happens every time James Zadina publishes a new paper or receives a write-up: the phone in his New Orleans laboratory begins to ring. The e-mails flood his in-box. The messages come from people all around the nation telling him how much they hurt.
“I get calls saying, ‘I have this terrible pain. When’s your medicine coming?’” Zadina says. “And my response is, ‘I can’t give it to you now. I’m working as fast as I can.’ That’s all I can say. But it’s difficult.”
For the last 20 years, Zadina, a researcher at the Tulane School of Medicine and the Southeast Louisiana Veterans Health Care System, has been on the front lines of a battle to defeat an ancient human adversary: physical pain. But lately his work has taken on new urgency. As opioid-related deaths and addiction in the United States reach epidemic proportions, Zadina has been attempting to engineer a new kind of painkiller that wouldn’t have the devastating side effects often caused by commonly prescribed drugs such as Oxycontin.
Researchers have been trying for decades to “separate the addictive properties of opiates from the pain-reducing properties.”
His pursuit is difficult because the very mechanisms that make those pills good at dulling pain are the ones that too often lead to crippling addiction and drug abuse. Like their close chemical cousin heroin, prescription opioids can cause people to become physically dependent on them. Researchers have been trying for decades to “separate the addictive properties of opiates from the pain-reducing properties,” says David Thomas, an administrator at the National Institute on Drug Abuse and a founding member of the NIH Pain Consortium. “They kind of go together.”
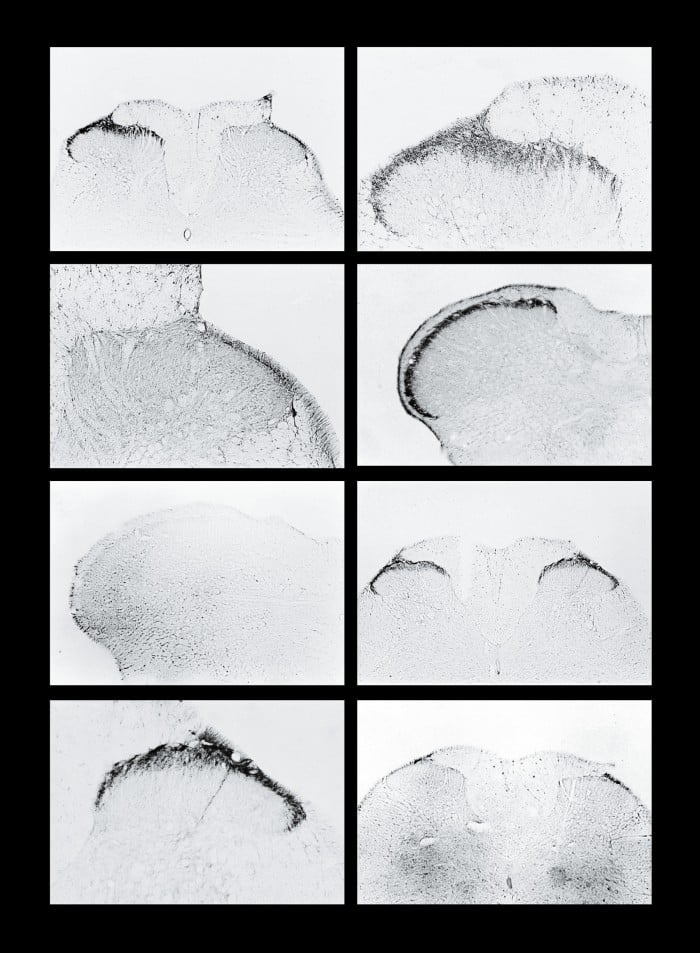
But Zadina believes he is getting close to decoupling them. Just this past winter, he and his team published a study in Neuropharmacology reporting that they had treated pain in rats without causing the five most common side effects associated with opioids, including increased tolerance, motor impairment, and respiratory depression, which leads to most opioid-related deaths. The next step is to test it in humans.
It’s just one of a number of efforts that aim to end the long-term damage that is being caused by relieving people of agony. Up to 8 percent of patients prescribed narcotic painkillers for chronic pain will become addicted, according to the National Institute of Drug Abuse. That’s why it used to be relatively difficult for patients to obtain opioids such as codeine to treat pain, Thomas says. That began to change in the 1990s. New opioids such as Oxycontin (and new marketing campaigns by pharmaceutical companies) arrived to meet the earnest demands of pain doctors and patient advocates who argued that many people with chronic pain—which afflicts an estimated 100 million Americans—were needlessly suffering.
But the pendulum has swung so far that opioids have become the default drug even when there might be better alternatives. Dan Clauw, director of the Chronic Pain and Fatigue Research Center at the University of Michigan, says that too many doctors now are essentially telling patients, “Well, I was taught that opioids would always work in any kind of pain, and if the pain’s bad enough and you’re desperate enough, I’ll try this class of drugs even if I am concerned about the risk of addiction.”
The consequences have been devastating. In 2014, the number of deaths from opioid overdoses in the United States topped 18,000, about 50 a day—more than three times the number in 2001. And that doesn’t even take into account painkiller addicts who have turned to heroin to soothe their cravings. Officials at the Centers for Disease Control and Prevention recently compared the scale of the problem to the HIV epidemic of the 1980s.
Developing any kind of better painkiller is very hard largely because pain takes complex pathways in our bodies. The signals that reach the brain and are interpreted as pain sometimes come from a problem on the periphery, or the surface, of our bodies, like when you get a cut. Other times the source of the pain signals is deeper: from damage to our nerves, which can happen with a really bad wound or, say, a back injury. And researchers such as Clauw are now finding evidence that much pain comes from a third type of situation: misfiring in the brain.
However, the presence of these different pain mechanisms also means there are a few different ways to try to solve the opioid problem. While Zadina and other scientists try to remove the dangerous properties from opioids, other new painkillers might target altogether different mechanisms in the body.
Make it stop
The main way to kill pain is simply to reduce the signals that the body feeds to the brain.
Nearly all our tissues have what are known as “nociceptive” nerve endings, tiny fibers whose job is to collect information and convey it back to the central nervous system and into the brain for processing. These fibers act as pain sensors. Some of the nerve endings respond to pressure, which causes them to send electrical impulses to the spinal cord so we actually feel hurt. Other kinds of nerve endings respond to changes in temperature, generating pain signals when things get too hot or cold. When we sustain an injury, inflammatory cells are recruited to the site and release at least a dozen different chemicals aimed at triggering other cells to come in and fight off pathogens, clean up debris, and begin rebuilding. But these inflammatory cells also cause the nerve endings at the site of the injury to fire more pain signals. In this type of localized injury, such as a sprained ankle or twisted knee, ice or anti--inflammatory drugs such as ibuprofen can be enough to tamp down the pain signals.
But sometimes—after a severe injury, an amputation, or diabetic nerve damage, for example—nerve fibers or the cells from which they originate physically change. Deep inside them, some genes can get turned on or off. That changes the number or type of active cellular machines known as sodium channels—proteins that stick out of the cells and regulate their ability to generate electrical impulses. Nerve cells talk to each other by means of these electrical impulses, and the sudden activity of extra sodium channels can cause a nerve to fire machine-gun-like bursts “spontaneously, even when there are no threatening stimuli,” explains Stephen Waxman, a professor of neurology at Yale University who directs the Center for Neuroscience and Regeneration Research at a Veterans Affairs hospital in Connecticut. Those bursts leave people in extreme pain. One common cause is chemotherapy. “Sometimes that pain is so bad people say ‘I can’t stand it,’” Waxman says. “‘I would rather die from cancer than have the pain associated with treatment.’”
“I’m working as fast as I can,” Zadina says. “That’s all I can say. But it’s difficult.”
There are nine kinds of sodium channels; the numbing medicine you get in the dentist’s office works by locally blunting all of them. That wouldn’t work as a general pain medication, because some of these channels are present in the brain and central nervous system. But Waxman is part of a cadre of researchers hunting for ways to target just one key sodium channel. He discovered its importance by studying people who have a rare genetic mutation that prevents them from making this particular channel. Even though the channel is not found everywhere in the human body, they essentially go through life feeling no pain. Conversely, people born with a hyperactive version of it feel as though “lava has been poured into their bodies,” Waxman says.
A drug developed by Pfizer, based on Waxman’s discoveries, has been tested on five patients, and similar painkillers are in development. Theoretically at least, these would not have major side effects.
Which brings us back to opioids.
Flipping a switch
Our peripheral nerves, where we pick up pain signals, lead back to the spinal column, where they connect with nerve cells that carry messages into the central nervous system and to neurons in the brain, at which point we feel the pain.
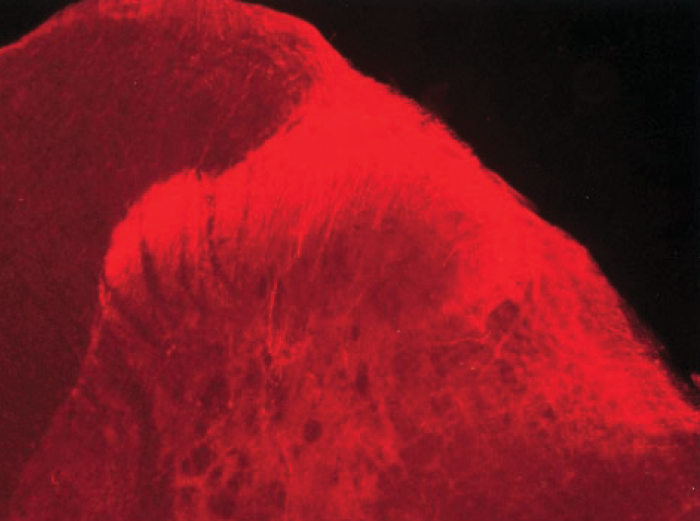
This is where all opioids, from Oxycontin to heroin and morphine, work their magic. They do so by binding to what are known as mu receptors at the junctions where nerve cells meet. That essentially flips a switch that reduces the ability of these cells to fire. So when nerve fibers at the periphery of the body send pain signals up to the brain for processing, the neurons that would normally make us feel this pain don’t respond.
“Opioids don’t touch the pain source; they only turn off the appreciation of the pain in the brain,” says Lewis Nelson, a professor of emergency medicine at New York University School of Medicine, who sat on a panel that recently recommended opioid guidelines for the Centers for Disease Control. “A small dose of an opioid just changes the sensation from being something that is quite irritating to being something that you don’t seem to care about as much.”
Mu receptors respond not only to painkilling drugs but also to “endogenous opioids,” natural signaling agents produced by our bodies—like the endorphins that are released during exercise, producing the so-called “runner’s high.” The problem is that the body doesn’t seem to respond to drugs such as heroin and Oxycontin in the same way it does to the endogenous substances.
Unlike endogenous opioids, pain drugs often activate specialized cells in the central nervous system, known as glia. Glia clean up cellular debris in the body and help regulate the response to injuries to the central nervous system. But when activated, they produce inflammatory substances—which can cause the body to register more pain signals. Many researchers, in fact, believe this increased activation of glial cells may be what causes the dangerous buildup of tolerance that makes opioids less effective over time, so that a patient needs higher doses to feel their effects. Eventually those higher doses can cause deadly respiratory problems.
All this might be avoided if Zadina can finally develop a synthetic opioid more like the body’s own substances—one that hits the mu receptors without activating glial cells. In the 1990s, he and his team isolated a previously undiscovered neurochemical in the brain, a pain-numbing substance they named endomorphin. He has been attempting ever since to perfect synthetic versions of it.
One of those versions was the drug that Zadina tested on rats in the study reported this past winter in Neuropharmacology. Like some of his previous compounds, this version appeared to be as good as or possibly better than morphine at relieving the animals’ pain without causing the worst side effects. Now he is in talks with several investors and biotech companies interested in turning it into a pill for people. Once he and his collaborators raise the money to start their own company, or ink a deal with a licensing partner, they intend to seek approval for early-stage human trials. “You never know until you actually put it in humans,” he says.
Some of Zadina’s experimental compounds have given rats as much pain relief as morphine.
Zadina’s drug would still be likely to activate the reward areas of the brain, and it might generate a mild high that could predispose some to addiction. But the rapid escalation of tolerance that opioids normally cause—and the physical withdrawal symptoms people endure when they stop taking them—would probably be removed from the equation. “I want to take away the dilemma that both patients and physicians face, of ‘Do I treat this pain adequately and risk addiction or do I treat the pain inadequately because I don’t want to use opioids?’” Zadina says. “That’s what drives me.”
But even if his new drug succeeds, neither it nor new sodium-channel painkillers are likely to treat a type of pain we weren’t even sure existed until recently—pain that does not seem to respond at all to opioids. Michigan’s Clauw has been studying this kind of pain for the past 20 years. From brain imaging studies, he has determined that it is caused by misfiring in the brain rather than a problem at the site where the pain seems to be coming from. He contends that this is the most common reason for pain in younger people suffering from conditions that have long confounded doctors, including fibromyalgia, certain headaches, and irritable bowel syndrome. What should those patients take instead of the opioids they are often prescribed? Many of them, Clauw argues, should be on drugs that can actually halt the misfiring by boosting neurotransmitters. Some drugs originally developed as antidepressants achieve this.
The NIH’s Thomas points to Clauw’s research as evidence that opioids today are simply overprescribed.
“If you get in a car accident, get wounded in battle, your arm gets blown up or something, and you’re in really severe pain, they will knock out severe pain pretty darn quickly,” says Thomas. “But right now they’re being used for all sorts of other cases where they’re probably not beneficial to the patient in the long run.”
Adam Piore is the author of The Body Builders: Inside the Science of the Engineered Human, which will be published in February.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.