Here’s how genes from covid-19 survivors could help you

Potential weapons against covid-19 include manufactured antibodies, serum transfusions from survivors, antivirals, steroids, and more than 100 vaccine candidates, some now advancing toward decisive tests in volunteers.
But there’s another approach to battling the virus—one that hasn’t won much attention, but which in the future could become the fastest way to beat back a pandemic. It involves isolating genetic material from survivors and injecting it directly into others, lending them protection against the pathogen.
DNA-encoded antibodies, as these therapeutics are called, have shown promising results in animals. In humans, genes injected into the arm or leg would convert the recipient’s muscle cells into factories to make antibodies against the virus. That could provide temporary immunity or lessen the severity of the disease for those already infected.
While no DNA-encoded antibody against covid-19 has yet reached human tests, laboratory experiments have started, says David Weiner, director of the vaccine and immunotherapy center at the Wistar Institute, who says his center has tested anti-covid gene injections on animals.
The use of conventional antibody drugs is one of the most promising treatment options for covid-19. Those drugs, however, must be produced in specialized bio-manufacturing facilities, which could limit their availability.
In contrast, gene therapy could offer a way to skip the complex and costly manufacturing of delicate antibodies and avoid the uncertainties involved in vaccines. As well, scientists say, gene injections can be used to carry information for more than one antibody at a time, which could stop a virus from developing resistance.
The advantage of the technique, researchers say, is its speed and low cost. DNA is manufactured in bacteria, which double in number every 30 minutes. “You can make DNA very readily, it’s dirt cheap, and you let the muscle make the antibody,” says Henry Ji, CEO of Sorrento, who says his company is exploring the idea with a partner, SmartPharm, of Boston.
Already in the works
Before the covid-19 pandemic, several universities and biotech companies were given tens of millions by DARPA, the US Defense Department’s science agency, to test the concept under a program to generate treatments against never-seen-before infections in 60 days.
In technology “sprints” organized by DARPA last year, teams at Wistar, Vanderbilt University, and the biotech firm AbCellera, among others, were asked to show whether they could develop an antidote to a known virus, such as Zika or pandemic H1N1 influenza, in two months. Each started with only with a blood sample from a survivor.
The process involved identifying an antibody to the pathogen in the survivor’s blood serum, isolating the genetic instructions to make it, and then injecting the DNA (or RNA) into mice. “We basically had a stopwatch to see how fast they could do the whole process,” says Amy Jenkins, who manages the program at DARPA.
At Vanderbilt, researchers live-tweeted their sprint to develop an anti-Zika shot. AbCellera, based in Vancouver, says that mice given a gene shot were able to survive a super-dose of avian influenza, 20 times the fatal amount. In both cases, antibodies made by muscle cells appear to have successfully stopped the infection.
DARPA had plans for a harder challenge in 2022, in which the teams would respond to a surprise virus chosen by the agency. But then the pandemic hit. “We didn’t have to give them a pathogen,” says Jenkins. “It found us, and it found us two years early.”
Spreading out your bets
In the rush that followed, DARPA’s planning proved useful, says Robert Carnahan, associate director of Vanderbilt’s vaccine center, since the groups were prepared to quickly locate convalescent antibodies from the blood of covid-19 survivors. Vanderbilt did so and sold the discovery to the pharmaceutical company AstraZeneca this April. In June, drug maker Eli Lilly said it would start testing antibodies found by AbCellera in covid-19 patients.
More on coronavirus
Our most essential coverage of covid-19 is free, including:
How does the coronavirus work?
What are the potential treatments?
What's the right way to do social distancing?
Other frequently asked questions about coronavirus
---
Newsletter: Coronavirus Tech Report
Zoom show: Radio Corona
See also:
Please click here to subscribe and support our non-profit journalism.
Those anti-covid antibodies will be made in bio-factories at great expense, and likely in limited supplies. Researchers say their idea for injecting the genetic information instead remains too novel for humanity to bet everything on. “The concept has been proven, but this is not a widely accepted technology—it’s nascent.” says Jenkins. “We are focusing on the sure bet, which is identifying antibodies and manufacturing them in the traditional sense.”
So far, injections of genetic material to turn muscles into antibody factories has been tried only two or three times in people. Only last year, Inovio tested the idea on volunteers in a Zika study using DNA injections. Moderna has tried it with RNA against the chikungunya virus. Scientific descriptions of the study results haven’t been published in either case.
Neither Inovio nor Moderna would tell MIT Technology Review whether they are advancing the gene therapy technique against covid-19. Both companies have vaccines in testing, and since the pandemic began, companies have learned that initiating human studies of covid-19 countermeasures can increase a company’s stock price by hundreds of millions. That means such information is closely guarded.
At Vanderbilt, Carnahan says the school has partnered with two biotech companies for work on DNA-encoded antibodies, but he declined to identify them.
One reason the gene therapy tactic may get backing is there are already more than 100 vaccines on the drawing board against covid-19, and many work in similar ways. “People have been going with proven technologies,” says May Pidding, business development director at Ichor Medical Systems, in San Diego. “But so many set their boats asail with a vaccine that now some may be thinking, ‘What else can we do to attack this?’”
Beyond the pandemic
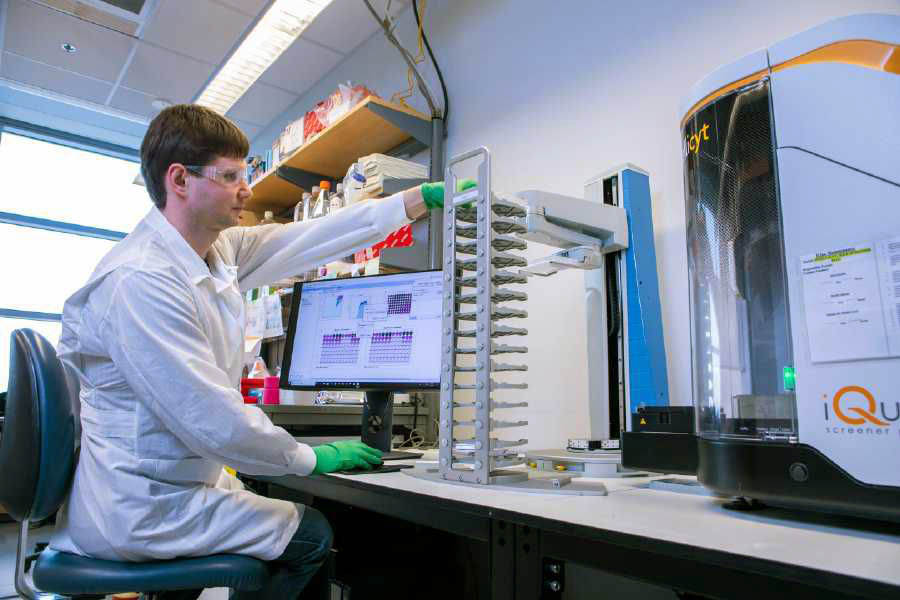
Ichor sells an electroporator—a device that delivers an electric shock, which causes muscle cells to open up for an instant and absorb the injected DNA. Pidding says a number of biotech firms have asked to use this gene gun, and she says some will try to deliver antibody genes.
Ultimately, some researchers say, the technique could play a role beyond fighting pandemics. According to Weiner, the genetic injections might also be an inexpensive way to deliver antibody drugs for cancer and arthritis. These are some of the top-selling but most expensive drugs on the market. A 2018 study found that the average cost for antibody drugs in the US was $96,000 a year.
As a result, some antibodies, like the cancer drug Herceptin, aren’t as widely used as they might be if they were cheaper. Researchers say DNA can be made at a small fraction of the cost of manufacturing antibodies. Whereas each antibody is manufactured differently, DNA “is always the same,” says Weiner. The molecule can also stay viable at room temperature for months.
Ji, the Sorrento CEO, thinks that DNA-encoded antibodies are a sure thing for the next pandemic, if not this one. “In the future, we will have gone through the drill,” he says. “You’ll just snap your gene in.”
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.