Personalized Medical Monitors
In late spring 2000, John Guttag came home from surgery. It had been a simple procedure to repair a torn ligament in his knee, and he had no plans to revisit the hospital anytime soon. But that same day his son, then a junior in high school, complained of chest pains. Guttag’s wife promptly got back in the car and returned to the hospital, where their son was diagnosed with a collapsed lung and immediately admitted. Over the next year, Guttag and his wife spent weeks at a time in and out of the hospital with their son, who underwent multiple surgeries and treatments for a series of recurrences.
During that time, Guttag witnessed what became a familiar scenario. “The doctors would come in, take a stethoscope, listen to his lungs, and make a pronouncement like ‘He’s 10 percent better than yesterday,’ and I wanted to say, ‘I don’t believe that,’” he says. “You can’t possibly sit there and listen with your ears and tell me you can hear a 10 percent difference. Surely there’s a way to do this more precisely.”
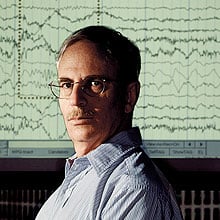
It was an observation that any concerned parent might make, but for Guttag, who was then head of MIT’s Department of Electrical Engineering and Computer Science, it was a personal challenge. “Health care just seemed like an area that was tremendously in need of our expertise,” he says.
The ripest challenge, Guttag says, is analyzing the huge amounts of data generated by medical tests. Today’s physicians are bombarded with physiological information–temperature and blood pressure readings, MRI scans, electrocardiogram (EKG) readouts, and x-rays, to name a few. Wading through a single patient’s record to determine signs of, say, a heart attack or stroke can be difficult and time consuming. Guttag believes computers can help doctors efficiently interpret these ever-growing masses of data. By quickly perceiving patterns that might otherwise be buried, he says, software may provide the key to more precise and personalized medicine. “People aren’t good at spotting trends unless they’re very obvious,” says Guttag. “It dawned on me that doctors were doing things that a computer could do better.”
For instance, making sense of the body’s electrical signals seemed, to Guttag, to be a natural fit for computer science. Some of his earlier work on computer networks caught the attention of physicians at Children’s Hospital Boston. The doctors and the engineer set out to improve the detection of epileptic seizures; ultimately, Guttag and graduate student Ali Shoeb designed personalized seizure detectors. In 2004, the team examined recordings of the brain waves of more than 30 children with epilepsy, before, during, and after seizures. They used the data to train a “classification algorithm” to distinguish between seizure and nonseizure waveforms. With the help of the algorithm, the researchers identified seizure patterns specific to each patient.
The team is now working on a way to make that type of information useful to people with epilepsy. Today, many patients can control their seizures with an implant that stimulates the vagus nerve. The implant typically works in one of two ways: either it turns on every few minutes, regardless of a patient’s brain activity, or patients sweep a magnet over it, activating it when they sense a seizure coming on. Both methods have their drawbacks, so Guttag is designing a noninvasive, software-driven sensor programmed to measure the wearer’s brain waves and determine what patterns–specific to him or her–signify the onset of a seizure. Once those patterns are detected, a device can automatically activate an implant, stopping the seizure in its tracks.
Guttag plans to test the sensor, essentially a bathing cap of electrodes that fits over the scalp, on a handful of patients at Beth Israel Deaconess Medical Center this spring. Down the line, such a sensor could also help people without implants, simply warning them to sit down, pull over, or get to a safe place before a seizure begins. “Just a warning could be enormously life changing,” says Guttag. “It’s all the collateral damage that people really fear.”
Now he’s turned his attention to patterns of the heart. Like the brain, cardiac activity is governed by electrical signals, so moving into cardiology is a natural transition for Guttag.
He began by looking for areas where large-scale cardiac-data analysis was needed. Today, many patients who have suffered heart attacks go home with Holter monitors that record heart activity. After a day or so, a cardiologist reviews the monitor’s readings for worrisome signs. But it can be easy to miss an abnormal pattern in thousands of minutes of dense waveforms.
That’s where Guttag hopes computers can step in. Working with Collin Stultz, a cardiologist and assistant professor of electrical engineering and computer science at MIT, and graduate student Zeeshan Syed, Guttag is devising algorithms to analyze EKG readings for statistically meaningful patterns. In the coming months, the team will compare EKG records from hundreds of heart attack patients, some of whose attacks were fatal. The immediate goal is to pick out key similarities and differences between those who survived and those who didn’t. There are known “danger patterns” that physicians can spot on an EKG readout, but the Guttag group is leaving it up to the computer to find significant patterns, rather than telling it what to look for. If the computer’s search isn’t influenced by existing medical knowledge, Guttag reasons, it may uncover unexpected relationships.
Joseph Kannry, director of the Center for Medical Informatics at the Mount Sinai School of Medicine, calls Guttag’s work a solid step toward developing more accurate automated medical readings. “It’s promising. The challenge is going to be in convincing a clinician to use it,” says Kannry.
Still, Guttag feels he is well on his way toward integrating computing into medical diagnostics. “People have very different reactions when you tell them computers are going to make decisions for you,” he says. “But we’ve gotten to the point where computers fly our airplanes for us, so there’s every reason to be optimistic.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.