The Search for a Perfect Male Birth Control Pill

Somewhere in Martin Matzuk’s collection of two billion chemicals, he hopes, is one that might safely make a man temporarily sterile—the elusive “male pill.”
Right now, male contraception means a condom or a vasectomy. But Matzuk, who is director of the Center for Drug Discovery at Baylor College of Medicine, is among a handful of scientists who are renewing the search for a better option—an easy-to-take pill that’s safe, fast-acting, and reversible.
Big drug companies long ago dropped out of the search for a male contraceptive able to chemically intercept millions of sperm before they reach a woman’s egg. But Matzuk’s lab shares in $600,000 worth of awards that the Bill and Melinda Gates Foundation gave out last year to “test the feasibility” of “disruptive and high-risk approaches” to male birth control.
That sum is pocket change next to the $147.9 million the same foundation spent in 2015 on family planning efforts aimed at women—efforts that it says reduce poverty. Scientists like Matzuk also think excessive population growth is a cause of scarcity and environmental degradation. “We just can’t sustain the population at the rate we’re going,” he says. A male pill could reduce the number of unintended pregnancies, which by one account make up 40 percent of all pregnancies worldwide.
“Right now the chemical burden for contraception relies solely on the female. That’s an unfair balance in the equation,” says Charles Easley, an assistant professor at the University of Georgia, who is also involved in the Gates-backed hunt for a male pill. “I think there’s not much activity in this field because we have an effective solution on the female side.”
To restart the search for a pill, Matzuk is beginning with lists of genes active in the testes and then creating mice that lack those genes. To do that, he’s working with researchers in Japan to use the gene-editing technology called CRISPR to snip out the genes one by one. Matzuk has so far made more than 75 of these “knockout” mice and says CRISPR makes the work much faster than it would be otherwise.
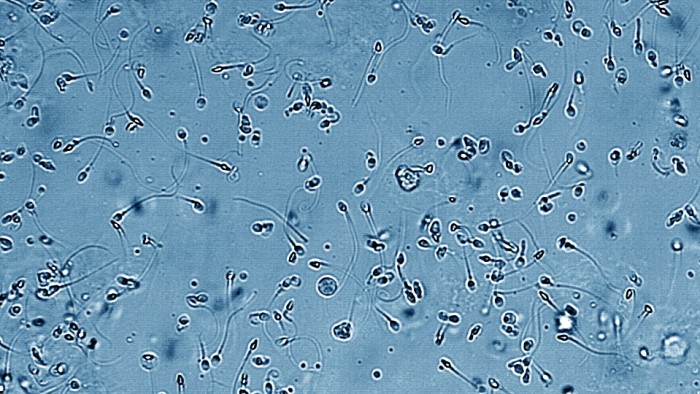
These mice are allowed to mate, and if their female partners don't get pregnant after three to six months, it means the gene might be a target for a contraceptive. Of 2,300 genes that are particularly active in the testes of mice, Matzuk has zeroed in on 30. His next step, he says, will be a novel screening approach to test whether any of about two billion chemicals can disable these genes in a test tube. Promising chemicals could then be fed to male mice to see if they cause infertility.
Female birth control pills use hormones to inhibit a woman’s ovaries from releasing eggs. But hormones have side effects like weight gain, mood changes, and headaches. A trial of one male contraceptive hormone was stopped early in 2011 after one participant committed suicide and others reported depression. And there’s another reason testing potential contraceptive drugs in male volunteers is tricky: some drug candidates have made animals permanently sterile. “The technical challenge is, how do we prevent sperm being made without permanently sterilizing an individual?” says Easley.
As a better way to test drugs, Easley is investigating yet another high-tech approach. He’s turning skin cells into stem cells that look and act like the sperm-making factory cells in the testes. Testing drugs on such human cells might provide more accurate leads than tests on mice, he thinks.
Any male pill would also have to start working quickly—maybe a lot sooner than the female pill, which takes a week. “As you can imagine, having a male contraceptive where you have to wait for it to work isn’t practical,” says Paul Andrews, director of operations at the National Phenotypic Screening Centre at the University of Dundee in the U.K.
Andrews and his team, also backed by Gates, use cameras to track how fast sperm swim and to capture what’s called the “acrosome reaction,” when sperm shed a cap-like structure before penetrating an egg. A drug able to immobilize sperm, or block that reaction, could be a starting point for an effective contraceptive, he says.
Scientists admit they’re facing a biological challenge. A man makes millions of sperm every day, while women’s ovaries usually release one mature egg each month. “You can’t really afford to have something that is 90 percent effective,” Andrews says. “It has to be 100 percent effective.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.