The Year in Biomedicine
Stem cells
In October, 12 years after human embryonic stem cells were first isolated, a therapy derived from such cells was tested in humans for the first time (First Human Tests of Embryonic Stem Cell Therapy Underway). The therapy, developed by Geron, is designed to treat spinal-cord injury with an injection of differentiated neural cells into the injury site.
Because the clinical trial is the first of its kind, Geron has had to forge a new path forward with the U.S. Food and Drug Administration as the agency figures out how to regulate embryonic-stem-cell therapies and assess the safety of these cells. The company initially won approval to begin clinical tests last year, but a few months later these were put on hold because animal tests raised new safety concerns.(FDA lets stem cell trials resume)
A second company, Advanced Cell Technology, won FDA approval in November to begin human tests of its embryonic-stem-cell-derived therapy for an inherited form of blindness.
While these two human trials mark major steps forward in stem-cell research, a federal judge in Washington, D.C., may have pushed the field a giant step back. In August, just 18 months after President Obama did away with an executive order from President George W. Bush’s administration that restricted the use of federal funds to a limited number of embryonic-stem-cell lines, Judge Royce Lamberth stunned the stem-cell community by issuing an injunction blocking federal funding for any research involving embryonic stem cells. (New Court Ruling Could Cripple Stem-Cell Research )
Researchers say the decision—even if it is later reversed—will have a damaging effect on the field, stunting promising medical research that was just building momentum. All grants under review at the nation’s largest funding agency, the National Institutes of Health (NIH), that involve human embryonic stem cells have been put on hold while the NIH and other government agencies try to get the injunction reversed.
The federal government quickly appealed the injunction, and an appeals court temporarily suspended it in September andheard the latest round of arguments in the case this month. It remains unclear how quickly that court will makes its decision, or when Judge Lamberth will make a final ruling.
In an ongoing effort to avoid the ethical battles that have stymied embryonic-stem-cell research, scientists developed a new method for making induced pluripotent stem cells, which are as flexible as embryonic stem cells but can be created from adult tissue without the use of embryos. (‘A New Way to Make Stem Cells’) The new method, developed by Derrick Rossi and collaborators at Harvard, is highly efficient and uses RNA instead of DNA to produce the four proteins needed to reprogram the cell. Eliminating the need for DNA bypasses some concerns in creating these cells, such as risk of growing tumors.
Genomics
This year, 10 years after the completion of the Human Genome Project, genome sequencing finally made its way into the practice of medicine. James Lupski, a physician-scientist who suffers from a neurological disorder called Charcot-Marie-Tooth, found the source of his disease after a 25-year search by sequencing his entire genome. (A Family Mystery, Solved by a Genome) Lupski’s research was the first to show how whole-genome sequencing can be used to identify the genetic cause of an individual’s disease
Scientists also are using sequencing to study and treat cancer, comparing the genomes of a patient’s healthy tissue and tumor tissue to identify the genetic mistakes that enabled the cancer cells to grow out of control. Steven Jones, Janessa Laskin, and collaborators at the British Columbia Cancer Agency used this approach to help select drugs for a man suffering from a rare adenocarcinoma. (Treating Cancer Based on Its Genome) Elaine Mardis and collaborators compared the genome sequence in a primary tumor and a metastatic tumor from the same patient to try to find mutations that allowed cells to break free from the original cancer site and spread through the body. (Genetic Clues to Cancer’s Spread) Foundation Medicine, a startup based in Cambridge, Massachusetts, aims to capitalize on these findings by creating a screening test capable of detecting variations in hundreds of cancer-linked genes. (Startup to Offer Patients a Genetic Profile of their Cancer)
Brain Control
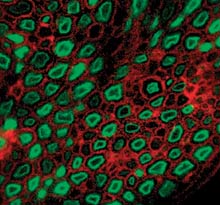
Optogenetics—the use of light to control genetically modified neurons—has rapidly become one of the hottest fields in neuroscience. Optogenetic technology is now in use in hundreds of labs across the globe, helping scientists gain insight into the brain. While the bulk of the research is focused in basic science, a handful of projects published this year point the way toward clinical applications. Researchers at Weill Cornell Medical College, in New York, developed a more accurate prosthetic retina for blind mice that had been genetically engineered to express a light-sensitive protein in certain retinal cells. (Now I See You) Gene therapy might one day make the same possible for humans.
Karl Deisseroth and colleagues at Stanford used optogenetic technology to control muscle movement in mice genetically engineered to express a light-sensitive protein in their peripheral nervous system. A tiny implantable LED cuff delivered millisecond pulses of light to the nerve, causing the animals’ leg muscles to contract. The researchers say that the light-triggered contractions mimicked normal muscle activity more closely than contractions generated by delivering electrical signals directly to the nerve. (Genetic ‘Light Switches’ Control Muscle Movement) The findings could aid in the development of nerve-stimulator devices that will help people paralyzed from spinal-cord injuries or disease.
To use optogenetics in the human brain, researchers need to figure out how to deliver light deep in the brain. Medtronic, one of the world’s largest medical-device makers, is working on just that. The company currently makes electrical deep-brain stimulators, which are approved to treat Parkinson’s and other neurological disorders. A similar device that delivers light rather than electricity could help improve the design of deep-brain stimulators, and might eventually become a therapy itself. (A Brain Implant that Uses Light)
Ed Boyden, one of the creators of the optogenetics, was featured in the October issue of Technology Review (Brain Control) and in a guest column online writes more about how science is co-opting nature’s ingenious solutions. (Defining an Algorithm for Inventing from Nature)
Synthetic Biology
Finally, Craig Venter and colleagues at the Venter Institute created life. (Synthetic Genome Reboots Cell, Making a Genome Quickly from Scratch) In the culmination of a 15-year project, researchers created a synthetic genome and then used it to reboot a microbial cell.
Using a method developed in 2008, the researchers, led by genomics pioneer Craig Venter, synthesized the genome of a tiny bacterium called Mycoplasma mycoides, containing just over a million DNA base pairs. Next they transplanted the synthetic genome into a related bacterium, Mycoplasma capricolum, in a process they had previously perfected using nonsynthetic chromosomes.
Once the recipient cells incorporated the synthetic genome, they immediately began to carry out the instructions encoded within the genome. The cells manufactured only M. mycoides proteins, and within a few rounds of self-replication, all traces of the recipient species were gone.
Venter and his colleagues are now working with Novartis and the National Institutes of Health to adapt the technology to quickly create vaccines against new strains of the flu virus.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.