Nanotech Revives a Cancer Drug
In the 1990s, a cancer drug called TNP-470 dramatically increased life span for some patients and led to complete cancer regression in others. But when neurotoxicity was detected in some patients, clinical trials were halted. This is a common problem: many drugs that show great promise in the lab fail in clinical trials due to unforeseen toxicity. Nanomedicine, however, promises a way to make safer, more effective versions of such drugs. Researchers at Children’s Hospital Boston have created and tested in mice a safer version of TNP-470.
“This is one of the first examples of nanotechnology resurrecting older drugs that we’re aware of,” says Piotr Grodzinski, director of the National Cancer Institute’s nanotechnology programs.
The resurrected drug, which has not yet reentered clinical trials, is well proven to be one of the most potent inhibitors of a process key to the spread of cancer. Most cancer deaths are caused by tumors that spread throughout the body, not by the original tumor. In order for these secondary tumors, which start with a single wandering cancer cell, to become entrenched and grow large enough to become deadly, they must first establish a network of blood vessels in a process called angiogenesis. If angiogenesis can be stopped, then a patient’s cancer won’t be able to spread. And compared with traditional chemotherapy and radiation, angiogenesis inhibitors have few side effects. The Children’s Hospital drug, called Lodamin in its nanoformulation, is “the most generic and potent angiogenesis inhibitor ever seen,” says Don Ingber, a professor of vascular biology at Harvard Medical School.
Ingber discovered the drug by accident in 1985, when he was a postdoc in the lab of Children’s Hospital researcher Judah Folkman. Ingber noticed that lab-grown blood-vessel cells accidentally contaminated with a fungus weren’t growing very well; an analog of the responsible fungal compound, TNP-470, was made by Takeda Pharmaceutical Company and extensively tested in animals. These studies suggested that it would prevent blood-vessel growth in a wide range of tumor types. Early-stage clinical trials of the compound were promising. In patients with lung cancer, says Ingber, the drug led to a 50 percent increase in life expectancy. But in some patients, the drug was a neurotoxin, causing confusion and dizziness and, in a few cases, more-serious problems. Just as TNP-470 was about to enter late-stage clinical trials, the company faced a lawsuit and stopped testing the drug.
But Folkman’s lab didn’t forget about TNP-470, even after another anti-angiogenesis drug, called Avastin, became a blockbuster. Avastin stops only one of the triggers of blood-vessel formation; TNP-470 works through an unknown mechanism but appears to target multiple parts of the process and, in animal studies, works in more tumor types. This broad activity suggests that it may work in more people, and that it should be difficult for tumors to become resistant to the drug. A few years ago, Folkman’s group modified TNP-470 to prevent neurotoxicity by attaching a large polymer that prevents the compound from crossing the blood-brain barrier. This version, however, must be given intravenously–a patient would have to return to the hospital again and again for treatments to prevent cancer recurrence.
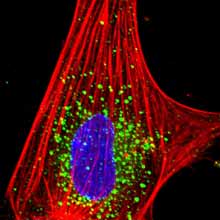
Folkman, who died in January, encouraged another researcher in his lab, Ofra Benny, to develop a version of TNP-470 that could be taken orally. Benny encased the drug in a micelle, a spherical polymer coating that resembles the fluff on a dandelion. The micelle, which is about 10 nanometers in diameter, is made up of two polymers that are both already FDA approved. Benny tested the new formulation, called Lodamin, in mouse models of melanoma and lung cancer. Her results, recently published in Nature Biotechnology, show that Lodamin is as effective as TNP-470–without having its toxicity. Hidden in the micelle, the drug is absorbed by the intestine into the bloodstream. First, it reaches the liver–a common site of secondary tumor growth–and then selectively accumulates in tumors throughout the body, inhibiting their growth.
The National Cancer Institute’s Grodzinski says that the potential for Lodamin to be taken orally is significant. “If it’s successful, that simplifies the treatment: you don’t have to come to the clinic to take it,” he says. The use of micelles for this purpose is novel, says Ingber, and could be applied to a range of other small-molecule drugs. Simple treatments with fewer side effects that keep small tumors from becoming dangerous are “the future for angiogenesis inhibitors,” he says, and will help cancer therapies keep pace with cancer diagnostics. “Early diagnosis is getting better, but we have nothing to offer these people.”
The group at Children’s Hospital is also developing Lodamin for other blood-vessel diseases, including some forms of blindness and arthritic pain caused by the invasion of capillaries into cartilage. Biotechnology company SynDevRx, based in Cambridge, MA, has optioned Lodamin for clinical development and is trying to bring it to clinical trials, says Ingber.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.