Inside Genomics Pioneer Craig Venter’s Latest Production
At Human Longevity Inc. (HLI) in La Jolla, California, more than two dozen machines work around the clock, sequencing one human genome every 15 minutes at a cost of under $2,000 per genome. The whole operation fits comfortably in three rooms. Back in 2000, when its founder, J. Craig Venter, first sequenced a human genome (his own), it cost $100 million and took a building-size, $50 million computer nine months to complete.
Venter’s goal is to sequence at least one million genomes, something that seems likely to take the better part of a decade, and use the data generated from them—along with information about some of the DNA donors’ health histories and the results of other medical tests—to find better ways to treat and prevent a range of disorders common among aging people, from cancer to heart disease.
Venter, 69, has raised $300 million from investors that include GE Ventures, the biotech company Celgene, and Illumina, which supplies the sequencing machines. And HLI has partnerships with the British pharmaceutical giant AstraZeneca and the South San Francisco–based Roche subsidiary Genentech, both of which are contributing patient samples for sequencing.
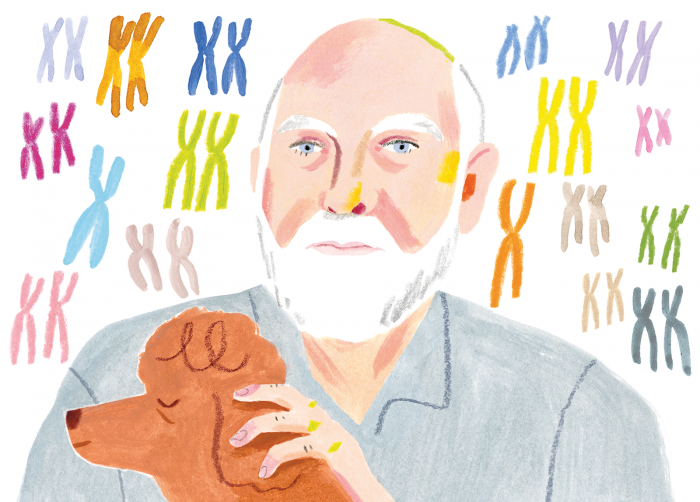
Seated behind his desk in his office two floors above the sequencing lab, his red poodle Darwin sleeping quietly at his feet, Venter has pulled up images on his computer that show how in one early experiment HLI scientists were able to sequence 1,000 people’s genomes and then reconstruct their faces solely on the basis of the genetic data. “We can predict your face, your height, your body mass index, your eye color, your hair color and texture,” he says, marveling at how closely one of the reconstructed faces matches the photo of the actual study participant.
But Venter says the ability to make faces out of genomes only hints at the full power of genetics. “Whether it’s the shape of your face, or a [diseased] aorta, or a narrowing of your spinal cord, we want to measure it so we can be able to predict those conditions in the future from the genetic code,” he says.
The understanding of genomics is still in its infancy, limiting the ability to draw firm links between genes and diseases. Even genes that have been well characterized don’t always lead researchers to medical breakthroughs. For example, Venter discovered he has a favorable variant in a gene called CETP (cholesteryl ester transfer protein) that had previously been associated with naturally healthy cholesterol levels and, by extension, a lower risk of heart attacks and strokes. In the early 2000s several pharmaceutical companies tried developing drugs to lower bad cholesterol levels by targeting a deleterious variant of the gene that leads to high levels of unhealthy cholesterol. They all failed.
“What that proves is that simple correlations don’t always work out. The whole field is learning there is complexity with this,” he says.
Venter is embracing the complexity, arguing that combining genomic information with other health data will unlock those links. Under the arrangement with AstraZeneca, the drug company will share 500,000 anonymous DNA samples from patients in its clinical trials with HLI, which will sequence and analyze the patients’ DNA. “Technology allows us to read every single letter of the genome, but the ability to detect sequence differences between hundreds of thousands of patients will make a huge impact in understanding both disease and drug response,” says Ruth March, who heads the pharma company’s initiative on personalized medicine and biomarkers. “HLI has the technology to spot patterns in data and build upon them, rather than just looking at random genes.”
To understand the health significance of each of the 20,000 or so genes in the human genome, scientists need to compare the genetic data with other information about the same people: data revealing how their genes are affected by environmental factors and behavior, records showing how they have responded to drugs, MRI images and other results from medical tests, and more. Only by discovering patterns among those data points, Venter believes, will HLI gain insights that physicians can use to practice “precision medicine,” tailoring treatment choices to the exact genetic makeup of each patient.
Correlating petabytes of genetic data with specific health conditions and then scanning for patterns among the million individuals whose genomes HLI is collecting is an enormous computing challenge. So Venter hired Franz Och, Google’s former machine-translation chief, who is best known for leading the development of Google Translate, software that translates any website in the world into English as quickly as any multilingual person can.
The challenge, says Och, is to correlate health conditions to the 6.4 billion letters that make up the genetic code. That code can be thought of as one language, MRI images as another language, and so forth.
For example, in people with Alzheimer’s, the hippocampus often shrinks years before they develop symptoms. Using machine learning to compare full genomes with brain images could uncover genetic variations that are related to Alzheimer’s risk. That might then yield targets for new drugs or early-detection devices. Or, says Och, it could reveal why some people with certain known genetic risk factors don’t get sick. “There might be other genetic changes that are protective,” he says.
“Whether it’s the shape of your face ... or a narrowing of your spinal cord, we want to measure it so we can predict those conditions.”
One of HLI’s major goals is to make cancer vaccines that are tailored to patients’ genetic makeup and that of their particular cancer. The idea would be to treat patients first, sequence their tumors as well as their entire genomes, and then give them a vaccine that would prevent their disease from coming back, says Ken Bloom, president of HLI and head of its oncology initiative. “It would prime the immune system and prepare it for another assault by the cancer, so it won’t recur,” Bloom explains.
Venter envisions a day when all of us will be able to have our genomes sequenced and used to improve our health care. He launched a prototype of that model in October 2015, called the Health Nucleus. Patients spend a day at the company’s La Jolla headquarters, getting their genome sequenced and undergoing medical tests. Health Nucleus customers, who pay $25,000 for the service, start their day in a private suite, decked out with leather chairs, discussing their family histories with a staff doctor for 90 minutes and having blood samples taken. Then they’re put through a battery of high-tech imaging tests that aren’t usually prescribed for healthy people, such as full-body MRI scans and 4-D echocardiography, which takes time-stamped pictures reflecting the full shape of the heart over time. They go home with a Band-Aid-size device on their chest that measures their heart rhythms for two weeks. All customers get access to a mobile app, where they can click on a 3-D avatar of themselves to learn which of their genes correlate to potential health conditions that might affect their heart, brain, and other vital organs. About 220 patients have signed up so far.
That approach has brought up a host of ethical and societal quandaries, says Arthur Caplan, a professor of bioethics at New York University’s Langone Medical Center, who has known Venter for many years and once worked as an advisor on one of his ventures. Who is going to pay for all this testing and personalized medicine? Is it even worth the money? Caplan points out that anybody who wants genome sequencing today has to pay out of pocket, because insurance companies rarely reimburse patients for genetic testing or counseling. So for now, at least, there’s an economic disparity in access to these highly tailored health regimens. “It’s only the rich who can pay right now for genome sequencing,” says Caplan.
That might be true for now, but Venter has hired actuaries to help prove out the economics of HLI’s personalized approach, hoping to get insurance companies on board. Even if it costs $25,000 per patient, he says, it beats spending hundreds of thousands of dollars on chemotherapy and other treatments that ultimately won’t save lives. “So $25,000 vs. hundreds of thousands of dollars, 40 years left to live vs. two years left to live,” he says. “How many of those cases do you need to say it’s more economical to prevent disease rather than just to treat it?”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.