Will Football Players Someday Take a Concussion Pill?
An experimental treatment helps restore normal brain structure and function in mice that have sustained severe concussions, and could lead to a drug that would do the same in humans, according to new research.
The brains of people who suffer from chronic traumatic encephalopathy (CTE), a progressive neurodegenerative disease that affects people such as boxers and football players with a history of repetitive hard hits to the head, are characterized by fibrous tangles of a protein called tau. It is not known how traumatic brain injury leads to these tangles, which are also found in the brains of people who suffered from Alzheimer’s disease.
Now researchers say they have identified a precursor to the tangles—a misshapen form of tau that appears in the brains of mice shortly after a blow to the head—and have shown that it can be eliminated by a protein, called an antibody, that binds to the misshapen tau and marks it for destruction by the body’s mechanism for clearing damaged or unneeded proteins. In mice that have sustained severe traumatic brain injuries like those commonly sustained by soldiers after a blast or by athletes after a blow to the head, the treatment prevents neurodegeneration and helps restore normal function. This suggests that the misshapen tau is a “major early driver of disease” after traumatic brain injury, say the researchers, and represents a promising drug target. The research was funded by the National Football League Players Association, the National Institutes of Health, and the Alzheimer’s Association.
Though the brains of individuals who had CTE are full of tau tangles, until now it has not been clear whether this “tauopathy” is a cause or a consequence of the post-traumatic neurodegeneration, says Kun Ping Lu, a professor of medicine at Harvard Medical School, who led the new research. He says this result confirms that it is a cause.
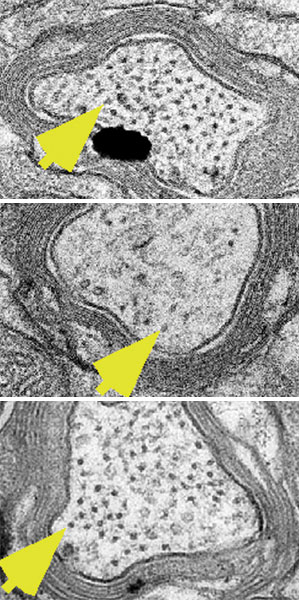
Normally, tau is important to the healthy function of neurons. Stress on the brain causes the protein’s structure to take two different shapes (see “A One-Two Punch for Alzheimer’s”). One form is needed for normal brain function. The other is a misshapen “bad guy” that leads to a disruption of neuron function that progressively spreads through the brain and leads to dementia and the loss of other important brain functions, and is prone to aggregation and tangling, Lu says.
Lu and his colleagues developed antibodies that bind to either the normal or misshapen tau only, and used them to study their relative levels in the brains of deceased football players and military veterans who had suffered from CTE. These brains contained large amounts of the misshapen version, whereas it was not present in normal brains.
To determine when the harmful protein appears, the researchers modeled sport and military-related traumatic brain injury in mice. Both severe brain injuries and mild, repetitive ones led to persistently high levels of the misshapen tau, which appeared as soon as 12 hours after a severe injury. Lu says he and his colleagues have observed that high levels of misshapen protein remain in the brain for many months following the injury.
After treating severely injured mice for two months, the animals showed minimal risk-taking behavior, whereas mice that did not receive the treatment showed a clear tendency to take risks, a hallmark of CTE that likely comes from neurodegeneration in brain regions important for high-level decision-making.
Lu says the near-term goal is to pursue an antibody-based diagnostic test that could detect harmful levels of the misshapen tau after a brain injury, potentially by measuring its presence in the blood. Beyond that, the goal is to “humanize” the mouse antibody, a fairly established process, he says, that could be accomplished within a couple of years. The result could be a drug that not only stops brain damage and prevents CTE after traumatic brain injury, but may also address tau-related pathologies that characterize Alzheimer’s as well as other neurodegenerative disorders, he says.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.