An Artificial Hand with Real Feelings
There have been remarkable mechanical advances in prosthetic limbs in recent years, including rewiring nerve fibers to control sophisticated mechanical arms (see “A Lifelike Prosthetic Arm”), and brain interfaces that allow for complicated thought control (see “Brain Helps Quadriplegics Move Robotic Arms with Their Thoughts”). But for all this progress, prosthetic limbs cannot send back sensory information to the wearer, making it harder for them to do tasks like pick up objects without crushing them or losing their grip.

Now researchers at the Cleveland Veterans Affairs Medical Center and Case Western Reserve University have developed a new kind of interface that can convey a sense of touch from 20 spots on a prosthetic hand. It does this by directly stimulating nerve bundles—known as peripheral nerves—in the arms of patients; two people have so far been fitted with the interface. What’s more, the implants continue to work after 18 months, a noteworthy milestone given that electrical interfaces to nerve tissue can gradually degrade in performance.
A video produced several weeks ago shows a 48-year-old Ohio man who lost his right hand in an accident three years ago using his prosthetic hand to pick up and remove stems from cherries without crushing them from excessive squeezing. This was thanks to the new technology, which allowed force detectors on the digits of his prosthetic hand to convey touch information directly to three pea-sized nerve interfaces surgically implanted in his lower right arm. He controls the hand through a standard technology called a myoelectric interface, which uses signals from the muscles in his lower arm to govern prosthetic hand movements.
The work opens up the possibility that prosthetic limbs could one day provide enduring and nuanced feedback to humans, says Dustin Tyler, the Case Western professor behind the project.
Lee Miller, a professor of neuroscience at Northwestern University who was not involved in the research, says the achievement appears remarkable. “This is the greatest number of distinct touch sensations generated by peripheral nerve stimulation that I know of, and the 18-month-long stability is also unsurpassed,” Miller says. A paper on the work is being prepared, Tyler says.
At the heart of the technology is a custom version of an interface known as a cuff electrode. Three nerve bundles in the arm—radial, median, and ulnar—are held in the seven-millimeter cuffs, which gently flatten them, putting the normally round bundles in a more rectangular configuration to maximize surface area.
Then a total of 20 electrodes on the three cuffs deliver electrical signals to nerve fibers called axons from outside a protective sheath of living cells that surround those nerve fibers. This approach differs from other experimental technologies, which penetrate the sheath in order to directly touch the axons. These sheath-penetrating interfaces are thought to offer higher resolution, at least initially, but with a potentially higher risk of signal degradation or nerve damage over the long term. And so they have not been tested for longer than a few weeks.
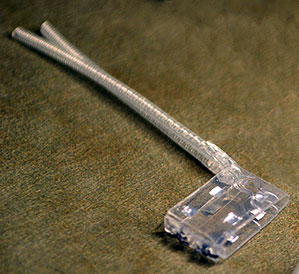
The cherry-grabbing test subject is Igor Spetic of Madison, Ohio. He lost his hand at his job when it was crushed in a drop-forging hammer while he was making an aluminum fitting for a jet engine. Now he’s got two small wiring harnesses protruding from a port in his upper right arm. At the lab, Tyler connects those harnesses to a device that generates the electrical signals that are sent to the cuff. This device, in turn, receives triggering information from sensors on his prosthetic hand.
His sensory feedback has only been felt in the lab so far, but Spetic professes amazement at his unique trial. “It’s real exciting to see what they are doing, and I hope it can help other people,” Spetic says. “I know that science takes a long time. If I don’t get something to take home, but the next person does, it’s all to the better.”
Researchers carefully place the implants to determine where Spetic perceives forces on his missing limb. Once installed, Spetic can detect sensations on several fingers and on the back and side of his missing hand, corresponding to inputs from the prosthetic. Once the implant is in place, the sensations always seem to arise in the same spots, and do not shift around, Spetic says.
Tyler can tune the electrical signals sent to the cuff to produce a variety of sensations. Spetic says sometimes it feels like he’s touching a ball bearing, other times like he’s brushing against cotton balls, sandpaper, or hair.
Tyler says the sensations Spetic reports are more natural and useful than the vague buzzing feeling that earlier experimental technologies had often produced. This means it may be possible to customize a sensation so that the patient feels like he’s touching a point of a pen, for example. Other groups and companies are working on better force detectors to attach to a prosthetic hand and generate such nuanced signals.
“[The] research is truly cutting edge and leading the world in terms of providing direct sensory feedback to amputees,” says Jack Judy, director of the Nanoscience Institute for Medical and Engineering Technology at the University of Florida in Gainesville. Judy recently served as a program manager for the Defense Advanced Research Projects Agency, where he ran a program that sought to improve the performance and reliability of neural interfaces used to control prosthetic limbs for soldier amputees. At least 1,715 soldiers suffered amputations in the wars in Iraq and Afghanistan.
Other existing technologies provide sensory inputs directly to nerves. Cochlear implants, for example, stimulate the auditory nerve to restore hearing, and technologies for stimulating the vagus nerve—which runs from the brain stem to the chest and abdomen—can be used to treat epilepsy and even depression. However, “when it comes to stimulating nerves to provide an effective sense of touch in humans, there has been far less progress,” Judy says.
There are other approaches to sensory feedback, including efforts to do this directly through brain implants (see “Giving Prosthetics a Sense of Touch”). But brain implants are considered farther off because of the heightened safety concerns from opening the skull. The Case Western work is in a pilot feasibility trial, and Tyler says that if all goes well, a device could be on the market in five to 10 years.
Deep Dive
Humans and technology
Building a more reliable supply chain
Rapidly advancing technologies are building the modern supply chain, making transparent, collaborative, and data-driven systems a reality.
Building a data-driven health-care ecosystem
Harnessing data to improve the equity, affordability, and quality of the health care system.
Let’s not make the same mistakes with AI that we made with social media
Social media’s unregulated evolution over the past decade holds a lot of lessons that apply directly to AI companies and technologies.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.