Safer Joint Replacements
Infections resulting from joint-replacement surgeries are costly and potentially deadly. Now researchers at MIT are developing coatings for medical implants that can be loaded with multiple drugs, including antibiotics that are released over time. The process involves layering antibiotic films, which are released over the short term, onto a permanently antibacterial polymer designed to prevent infection over the long term.
About one percent of knee and hip replacement surgeries result in infection; the number rises to three to five percent for second surgeries. “It’s a low rate, but if you are the one out of one hundred who gets an infection, the complications are catastrophic,” says Lloyd Miller, assistant professor of orthopedic surgery at the University of California, Los Angeles. All the infected tissue and hardware must be surgically removed and replaced with an antibiotic block; the patient cannot walk for six to eight weeks while being treated with intravenous antibiotics to eliminate all traces of infection; and then a revision surgery is done. Complications due to infection are also enormously expensive. A joint replacement costs about $30,000 in the United States, but dealing with infections can raise the tab to nearly $150,000.
Most infections happen when bacteria enter the body with an implant. But artificial joints can become infected years later when bacteria are introduced into the bloodstream during dental work, colonoscopies, and other procedures, says Miller, who is not affiliated with the MIT group. Orthopedic coatings that have permanent antibacterial properties in addition to a transient coating of antibiotics could keep patients protected.
Although antibiotic coatings for many other medical devices have already been developed, coatings for joints pose particular challenges. Unlike stents and other devices that are static, joints have to be able to move. So the coating can’t be too thick, and it mustn’t interfere with joint articulation.
Researchers led by Paula Hammond, professor of chemical engineering at MIT, are using a polymer-coating technique called layer-by-layer assembly to load large concentrations of drugs into implant coatings without making them too thick. Hammond’s group builds up these films by dipping an implant alternately in solutions of negatively and positively charged molecules such as polymers and drugs. The difference in surface charge holds each layer tightly to those above and below it. This process leads to very thin layers of materials, on the order of tens of nanometers thick. The drugs will be released when the polymers biodegrade inside the body.
Alternating layers of drugs with layers of a biodegradable polymer, rather than mixing polymer and drug and slathering the mixture on an implant, results in a thinner coating that contains a higher proportion of the drug—as much as 50 percent, rather than the more usual 4 percent. And these coatings can be produced at low temperatures and in water, rather than in the harsh conditions usually required for polymer processing. This means they’re compatible with a broader range of delicate molecules including protein drugs and therapeutic RNA.
“What distinguishes this technology is the promise of being able to release different drugs sequentially, in a controlled way,” says Myron Spector, professor of orthopedic surgery at Harvard Medical School. Patients who have a poor vascular system that can compromise bone growth, including diabetics and heavy smokers, might benefit from coatings that release drugs to stimulate bone formation or blood-vessel growth, in addition to antibiotics.
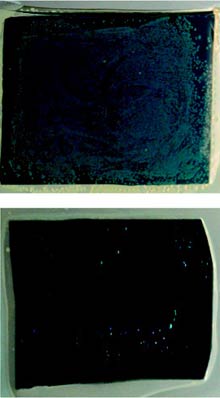
The permanent layer of antimicrobial polymer on which Hammond builds the drug-releasing films was previously developed by Alexander Klibanov, a professor of chemistry at MIT. “When these polymers are present on a surface, bacteria will die on impact—the polymer disrupts the cell membrane, and the bacteria’s guts spill out,” says Hammond. When submerged in a solution of staph bacteria for two weeks, a different substrate untreated with the layers of antibiotics was completely colonized by bacteria by the end of the first hour. No bacteria took hold on a surface of Klibanov’s polymer treated with Hammond’s films over the two-week period, even after the drug-releasing layers degraded. This work was published online in the Journal of the American Chemical Society in November.
Spector has worked with Hammond on preliminary studies of the coatings in animals and will now work with the MIT group to demonstrate whether they do improve outcomes after a joint replacement. Miller of the University of California, who has worked on antimicrobial implants in animals, notes that many factors remain unknown. For example, “we don’t know for how long we want a drug to be released,” he says. Further tests should make this clearer.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.