Biosensors Comfortable Enough to Wear 24-7
Many medical sensors, like the sort used for heart-monitoring electrocardiograms (ECGs) or brain-monitoring electroencephalograms (EEGs), require direct skin contact and a sticky layer of gel to help conduct electrical signals. Both technologies can be remarkably precise, but they don’t transfer easily from hospital to home. Now researchers at the University of California, San Diego believe they may have solved the sticky situation with a sensor that can read ECG and other data through clothing, without ever touching the skin.
Scientists have had a tough time developing something that can reliably detect the skin’s polarity changes without direct contact. ECG electrodes detect the time it takes for waves of changing polarity (caused by heart-muscle contractions) to travel to different sensors, which reveals the electrical activity of different parts of the heart. Currently, these sensors require a gel or an allergy-inducing adhesive. Nonsticky or “dry” sensors are uncomfortable and particularly sensitive to motion, so they can’t be used outside the clinic or for long periods of time.
Instead of using electrodes, the UCSD researchers built a capacitive sensor, which conducts much weaker signals but can do so across small distances. While the concept goes back decades, prior attempts at building such sensors have been impractical for mass production–they tended to be either too costly, too sensitive to outside noise, or both. The sensor developed by bioengineer Gert Cauwenberghs and his graduate student, Mike Chi, uses off-the-shelf components and clever circuitry to get around these problems. The resulting sensor can detect faint changes in capacitance, and amplify them, while canceling out the ambient electrical noise that exists all around us. “What’s out there today requires several discrete components,” Chi says. “Our process makes it reliable and inexpensive, so we have a circuit that can be mass-produced.”
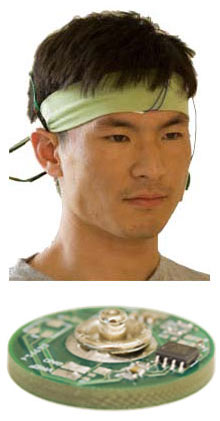
Chi’s sensor is barely larger than a quarter, and when multiple sensors are embedded in material and wired together, they create a portable monitor that patients can wear over clothing as they go about their daily routine. This could mean increased monitoring time and better compliance from patients.
Currently, when cardiologists want to know what a patient’s heart activity looks like for an extended period of time, they have to send them home with a Holter monitor, a portable ECG device that employs the same wired, sticky electrodes used in the hospital. But this monitor can only be used for up to 48 hours, and abnormal cardiac rhythms don’t always occur during such a short window of time. “A lot of these events are transient, and with today’s tech you actually miss the events because you can’t capture them reliably,” Chi says. If a patient could wear a vest over his clothing, such monitoring could go on for as long as a physician required.

Incorporating the sensors into a headband makes it possible to monitor some electrical activity in the brain, too. “For a one-time doctor visit with ECG and EEG, it probably doesn’t matter whether you [use sticky-sensors] or not. But for long-term use, that definitely makes a difference,” says Maysam Ghovanloo, a bioengineer at the Georgia Institute of Technology.
The UCSD group is collaborating with a group at Oregon State University to create a completely wireless version of its sensor, with a Bluetooth transmitter that can relay information to a receiver. “I think what they’re doing is a really important contribution,” says Eric Topol, director of the Scripps Translational Science Institute in San Diego and a specialist in wireless health. “I think it’s very viable and attractive, and it’s a welcome addition to the wireless sensor tool kit.”
Long-term, Chi and Cauwenberghs hope that the sensors could also be helpful for advancing brain-computer interface applications. “We wanted to build a very sensitive sensor that can acquire signals reliably through hair without any messy gels or abrasion or any preparation. Something that’s easy to use and very quick,” Chi says. Such sensors could be used to help spinal-injury patients communicate, or even be combined with gaming systems.
But while the EEG sensors can pick up certain brain activity, the sensors must be made more sensitive, as neural activity in the brain is remarkably faint. “Noncontact electrodes are going to be an advantage no matter where you put them on the body,” says Rahul Sarpeshkar, a bioelectronics engineer at MIT. “But all of these systems, when applied in medicine, have to deal with motion and the strength of a signal, which makes the EEG more technically challenging.”
Cardiac applications may be closer at hand: Chi and Cauwenberghs have data showing that their sensors can pick up signals that are nearly as accurate as those collected using gel-based electrodes. Chi is creating a startup company, Cognionics, to develop the sensors further, and has already begun talks with medical-device companies.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.