Human Heart Grows New Cells
The human heart has a notorious reputation for being unable to heal itself, but new research suggests it is capable of at least some self-repair. Using carbon dating to gauge the age of heart cells, scientists have found that low numbers of new heart cells are continuously being created throughout a person’s life. This raises the possibility that we may one day be able to use drugs to directly stimulate this regenerative capacity to patch up damaged hearts, rather than relying on cell-transplantation therapies.
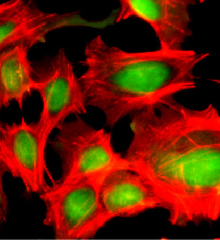
Scientists can make new cardiomyocytes–heart muscle cells–from stem cells in cell-culture experiments, and evidence for cardiac stem cells has been building. But it was unclear until now whether new heart muscle cells are ever born under real-life conditions inside the heart after birth.
Ratan Bhardwaj and his colleagues at the Karolinska Institute in Stockholm, Sweden, used radiocarbon dating, which is normally employed to establish the age of archaeological or geological remains, to work out the age of heart cells compared to the chronological age of the person from which they were isolated. To do this, the team took advantage of nuclear tests done during the 1950s and 1960s, which led to a sharp increase of radioactive Carbon 14 in the atmosphere. The radioactive material was captured by plants as CO2 and then worked its way up the food chain and into the DNA of the human body. Soon after the tests were stopped, atmospheric C14 levels declined again, leading to a corresponding drop in the C14 concentration in human DNA.
The team measured C14 levels in the heart tissue of twelve deceased patients aged between 19 and 73 at the time of death and found elevated C14 even in those subjects who had been born two decades before the nuclear tests started, indicating that the radioactive carbon must have been incorporated into heart muscle cells long after birth. Similarly, the C14 levels in the hearts of younger patients did not match the year of their birth but rather indicated a younger birthday for the cells. The research was published today in the journal Science.
“I am very excited about how they have used this novel technology to get something useful out of such a terrible environmental disaster,” says Charles Murry, director of the Center for Cardiovascular Biology at the University of Washington in Seattle, who coauthored a commentary, also in Science, on Bhardwaj’s research.
According to the findings, heart muscle cell turnover is slow compared to other types of cells and decreases with age. Using mathematical modeling, Bhardwaj and colleagues worked out that only 1 percent of cells are typically exchanged per year in young adults. This rate drops to only 0.4 per cent by age 75. This means that a 55-year-old will have rebuilt 45 per cent of her heart since birth. Other cells in the heart, such as those that form connective tissue and blood vessels, renew much faster, exchanging about 18 percent every year. Just why muscle cell turnover should be so slow remains unknown.
Bhardwaj and Murry both say that the discovery holds great therapeutic potential if a drug can be found to stimulate increased renewal of heart cells: “A lot of us have been working on putting exogenous cells [cells from a donor or other parts of the body] into the heart,” says Murry. “But given the choice of growing my own heart back or taking all these cells from elsewhere, I would choose the pharmaceutical approach.” No such drug has been identified to date.
Not everyone agrees that a pharmaceutical approach is the best option, however. “A drug may stimulate a biochemical pathway too crudely, and in regenerative medicine, we need to be very careful to avoid unregulated cell growth that could cause tumors,” says Joshua Hare, director of the Interdisciplinary Stem Cell Institute at the University of Miami Miller School of Medicine. Hare argues that the best approach would be to identify and purify cardiac stem cells from the patient and amplify them in cell culture, then put them back into the body in a controlled way. Some scientists are already investigating such an approach.
But Hare also thinks there may be a third way to harness the renewal power of the heart’s own cells. He is currently developing therapies that aim to heal heart injuries with stem cells obtained from bone marrow. “It may be that injecting these cells could also boost the activity of cardiac stem cells,” he says.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.