More than 200 people have been treated with experimental CRISPR therapies
But at a global genome-editing summit, exciting trial results were tempered by safety and ethical concerns.

This article is from The Checkup, MIT Technology Review's weekly biotech newsletter. To receive it in your inbox every Thursday, sign up here.
I’ve spent the last few days thinking about how, when, and if we should use gene-editing tools to change the human genome. These are huge questions, and very emotive ones—especially when it comes to editing embryos.
I watched scientists, ethicists, patient advocacy groups, and others wrestle with these topics at the Third International Summit on Human Genome Editing in London earlier this week.
There’s plenty to get excited about when it comes to gene editing. In the decade since scientists found they could use CRISPR to edit cell genomes, multiple clinical trials have sprung up to test the technology’s use for serious diseases. CRISPR has already been used to save some lives and transform others.
But it hasn’t all been smooth sailing. Not all of the trials have gone to plan, and some volunteers have died. Successful treatments are likely to be expensive, and thus limited to the wealthy few. And while these trials tend to involve changes to the genes in adult body cells, some are hoping to use CRISPR and other gene-editing tools in eggs, sperm, and embryos. The specter of designer babies continues to loom over the field.
It was at the last summit, held in Hong Kong in 2018, that He Jiankui, then based at the Southern University of Science and Technology in Shenzhen, China, announced that he had used CRISPR on human embryos. The news of the first “CRISPR babies,” as they became known, caused a massive ruckus, as you might imagine. “We’ll never forget the shock,” Victor Dzau, president of the US National Academy of Medicine, told us.
He Jiankui ended up in prison and was released only last year. And while heritable genome editing was already banned in China at the time—it has been outlawed since 2003—the country has since enacted a series of additional laws designed to prevent anything like that from happening again. Today, heritable genome editing is prohibited under criminal law, Yaojin Peng of the Beijing Institute of Stem Cell and Regenerative Medicine told the audience.
There was much less drama at this year’s summit. But there was plenty of emotion. In a session about how gene editing might be used to treat sickle-cell disease, Victoria Gray, a 37-year-old survivor of the disease, took to the stage. She told the audience about how her severe symptoms had disrupted her childhood and adolescence, and scuppered her dreams of training to be a doctor. She described episodes of severe pain that left her hospitalized for months at a time. Her children were worried she might die.
But then she underwent a treatment that involved editing the genes in cells from her bone marrow. Her new “super cells,” as she calls them, have transformed her life. Within minutes of receiving her transfusion of edited cells, she felt reborn and shed tears of joy, she told us. It took seven to eight months for her to feel better, but after that point, “I really began to enjoy the life that I once felt was just passing me by,” she said. I could see the typically stoic scientists around me wiping tears from their eyes.
Victoria is one of more than 200 people who have been treated with CRISPR-based therapies in clinical trials, said David Liu of the Broad Institute of MIT and Harvard, who has led the development of new and improved forms of CRISPR. Trials are also underway for a range of other diseases, including cancers, genetic vision loss, and amyloidosis.
Liu highlighted the case of Alyssa, a teenager in the UK who was diagnosed with a form of leukemia that affects a type of white blood cells called T cells. Chemotherapy didn’t work, and neither did a bone marrow transplant. So doctors at Great Ormond Street Hospital in London tried a CRISPR-based approach.
It involved taking healthy T cells from a donor and using CRISPR to modify them. The treated cells were altered so that they wouldn’t be rejected by Alyssa’s immune system, but they would be able to track down and attack Alyssa’s own cancerous T cells. These cells were then given to Alyssa as a treatment. It seems to have worked.
“As of now, approximately 10 months after treatment, her cancer remains undetectable,” Liu said.
It really is incredible that we are hearing such success stories already. But there are concerns.
The question of equity came up again and again at the summit. Gene-editing therapies are expected to cost a lot of money—likely millions of dollars. Who will be able to afford them? Probably not the people living in low- and middle-income countries, multiple attendees worried.
For now, CRISPR therapies are still considered experimental, and none have been approved, so the only way for people to access them is through clinical trials. The majority of these are being run in the rich world. Natacha Salomé Lima, a psychologist and bioethicist at the University of Buenos Aires in Argentina, pointed out that while 70% of global cancer cases are in low- and middle-income countries, two-thirds of gene-therapy cancer trials are taking place in wealthy countries.
I could tell that the summit’s organizers had made an effort to feature speakers from all over the world, and to include people who have the disorders being targeted by gene editing. But some attendees felt that some voices were still missing from the discussion. “What about the LGBTQ community?” Marc Dusseiller of ETH Zurich in Switzerland, who describes himself as a “workshopologist” interested in biohacking and bio art, asked me.
It’s also worth pointing out that not all CRISPR treatments have been a success. Multiple researchers noted that we still don’t fully understand how the treatment works. We know we can cut DNA, and swap either DNA bases or chunks of genetic code. But we can’t be sure about unintended effects elsewhere in the genome. It’s possible that you could accidentally trigger some genetic change elsewhere—one that might have harmful consequences.
Last year, 27-year-old Terry Horgan died while participating in a clinical trial of a CRISPR treatment designed to treat his Duchenne muscular dystrophy, a fatal disease that causes muscle degeneration. The cause of his death—and whether or not it might have been related to the treatment—has not been made clear.
And there’s always a risk that rogue scientists will set up companies offering unapproved procedures to desperate individuals who are willing to pay for them, said Robin Lovell-Badge, a stem-cell biologist at the Crick Institute, where the summit took place. They might even sell unauthorized procedures designed to enhance people rather than treat them.
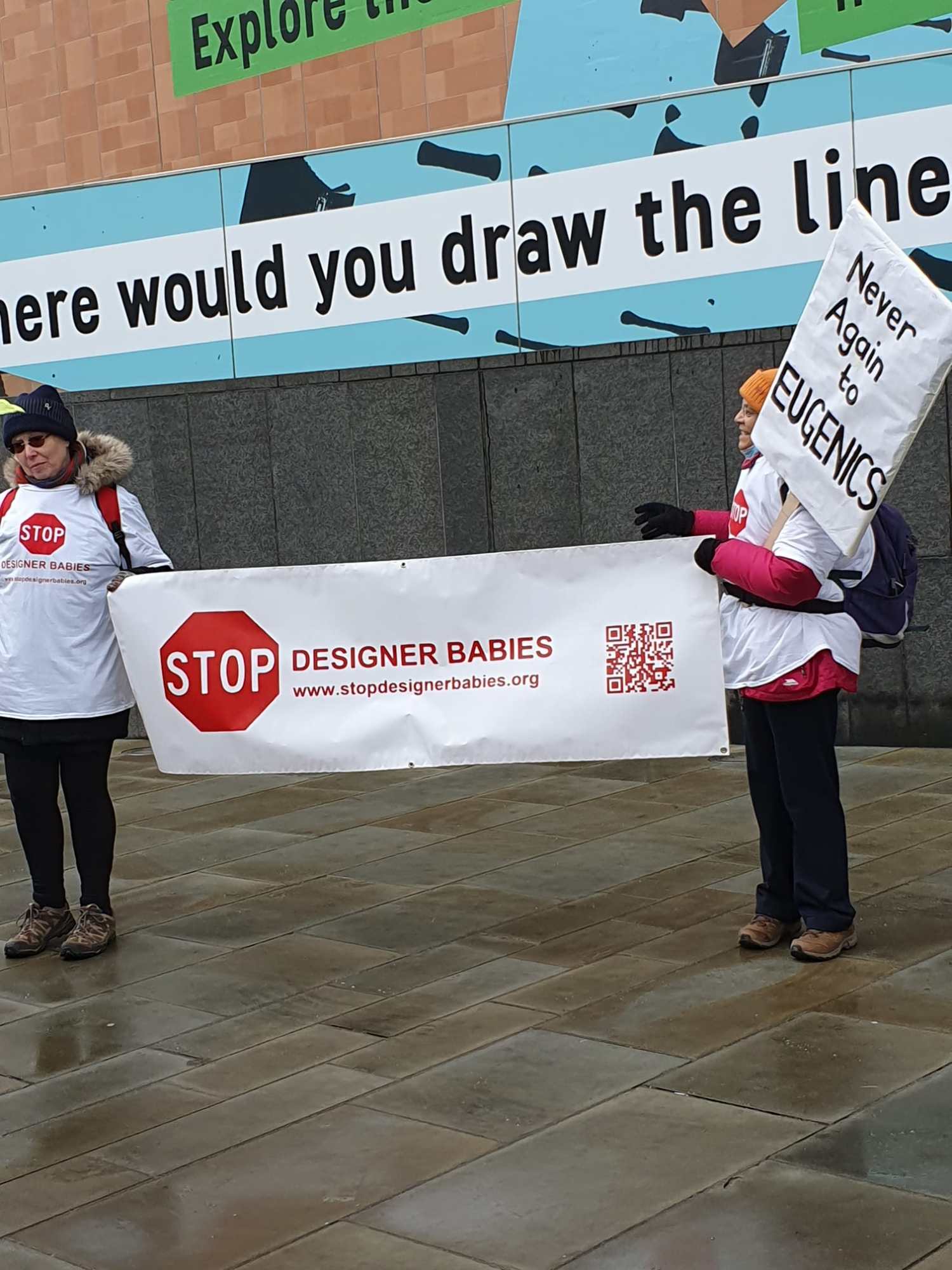
On the first day of the summit, a couple of protesters stood at the entrance of the venue, holding a banner reading “Stop designer babies.” This sentiment is shared by a lot of scientists. They are particularly worried about future attempts to edit the genes of eggs, sperm, or embryos.
In theory, you could change the DNA of an embryo to prevent a baby from developing a heritable disease. But research into early embryos (scientists are generally allowed to study them for only 14 days before having to destroy them) suggests that they are even more likely to be affected by unintended, potentially harmful effects of gene editing. And these changes would be passed on to the next generation, too.
Most attendees focused on technical and ethical worries, but Dusseiller had another concern. The summit was too dry, he told me; the serious issues surrounding gene editing can be addressed with some degree of humor. “We need more weirdness,” he argued. “We need more jokes.”
Read more from Tech Review's archive
There are more than 50 experimental studies underway that use gene editing in people to treat cancer, HIV, blood diseases, and more. Most of them involve CRISPR, my colleague Antonio Regalado reported earlier this week.
And last year, a volunteer in New Zealand became the first to receive an experimental CRISPR treatment to lower her cholesterol. One of the scientists behind the work thinks the approach could potentially benefit almost everyone.
CRISPR is also being explored for an inherited form of blindness. The first volunteer underwent the experimental treatment in 2020.
He Jiankui’s work was never published. It was rejected by the leading medical journals it was submitted to. But Antonio got hold of the manuscript, and showed it to four experts. Their verdicts were damning. He’s claims were not supported by his results, the babies’ parents may have been under pressure to agree to join the experiment, and the researchers went ahead without fully understanding what they were doing.
The summit was focused on human genome editing, but CRISPR is also being explored to make farmed animals bigger and stronger. One team of scientists has put an alligator gene into catfish in an attempt to make them more resistant to disease, for example.
From around the web
A microbiologist found a forgotten beef soup at the back of her fridge had turned bright blue. So she set out on a scientific quest to find out why. (Twitter)
Governments around the world are using algorithms to control access to various services. A system that flags people who might be committing benefits fraud in Rotterdam appears to discriminate on the basis of ethnicity and gender, according to an investigation. (Wired)
Last year, biotech company Retro Biosciences announced its launch with $180 million in funding. It turns out that all of that is from Sam Altman, the CEO of OpenAI. (MIT Technology Review)
Makena, a drug approved to prevent preterm birth, has been voluntarily pulled from the market by the company that makes it. Several studies have shown that the drug doesn’t work, and the US Food and Drug Administration recommended that it be withdrawn back in 2020. (The New York Times)
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.