The US is launching a trial for blood tests that promise to catch cancers earlier
Dozens of these tests exist, but so far none have earned FDA approval.
Most cancers can’t be reliably screened for before symptoms begin—tools like mammograms and pap smears are exceptions, not the rule. To improve detection, dozens of companies have designed single tests to spot signs of multiple kinds of cancer in blood drawn from a patient’s arm. Now, a national trial is preparing to launch in the US to see how good these tests actually are.
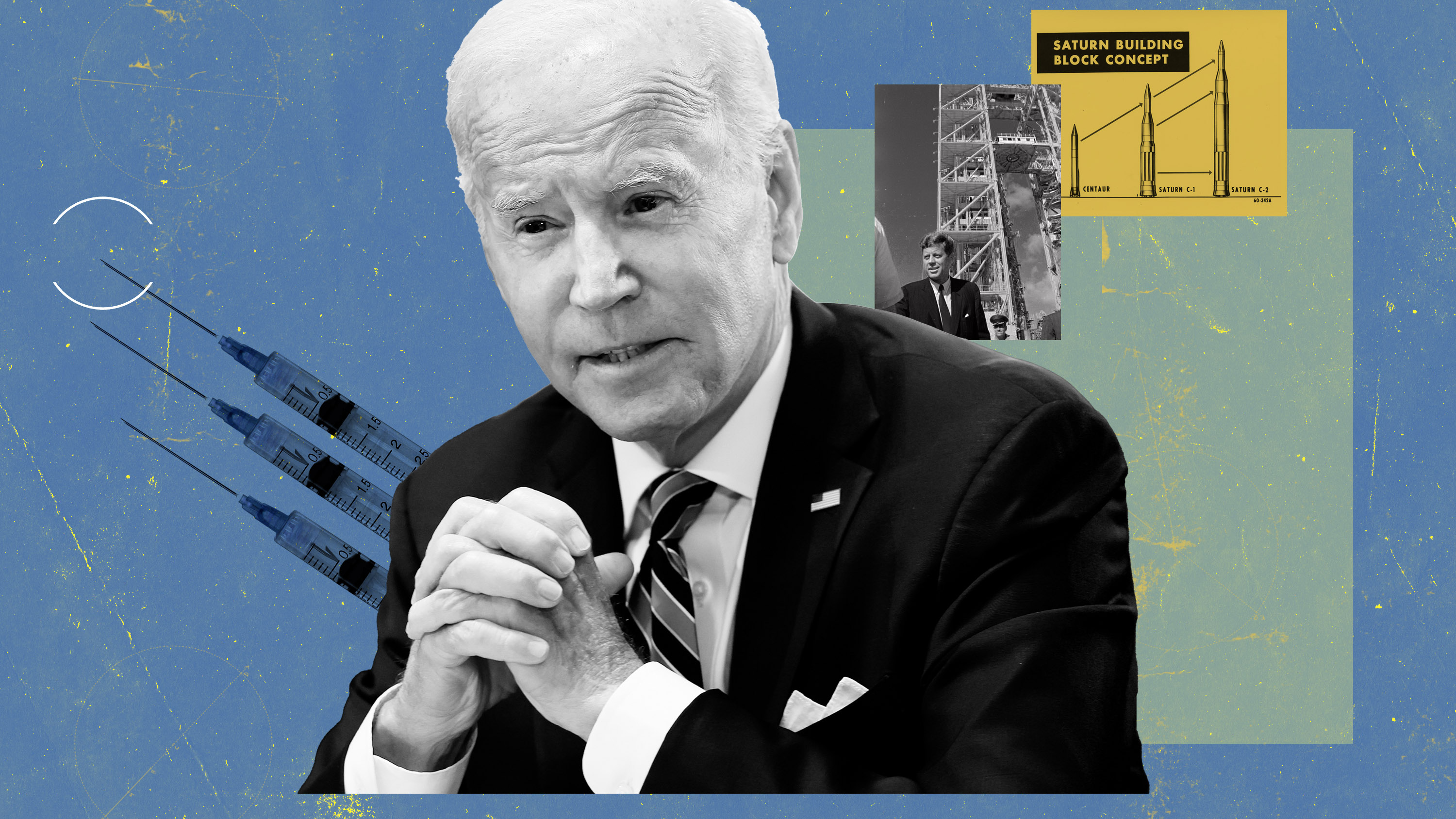
In a speech on Monday in Boston, President Biden highlighted these new blood tests and the upcoming trial as central to the Cancer Moonshot—a federal push to halve US cancer deaths in the next 25 years. Biden’s speech came on the 60th anniversary of President John F. Kennedy’s speech pledging to bring a man to the moon and back—the inspiration behind this latest moonshot.
The new trial, run by the National Cancer Institute, will begin enrolling participants in 2024 and test how effective various blood tests are at spotting cancer in 24,000 healthy patients over four years. If the findings seem promising, a clinical trial almost 10 times as large will commence.
Most of these multi-cancer early detection tests, or MCEDs, work by looking for remnants of tumor cells that explode after the immune system attacks them. Debris from dead tumors turns up in the bloodstream, where it can potentially be detected to warn of cancer before someone feels sick. If imaging confirms the finding, a biopsy follows.
Only one of these tests is currently being used in the US. The Galleri, which claims to detect over 50 cancers, is available with a prescription for $949. But since it lacks FDA approval, it’s not covered by most insurance. New data released by its developers shows that the test caught cancer in 35 people out of a pool of about 6,600 believed to be healthy—and 26 of the cases it caught were cancers not routinely screened for.
Questions remain about how to interpret MCED test results. Only some blood tests can pinpoint which organ the cancer is actually in. Lab tests must be run on potentially cancerous tissue to confirm a diagnosis, but you can’t biopsy someone’s entire body. False positives remain an issue for the entire field of cancer screening, which, by design, involves sifting through mounds of healthy tests to find cancer. Galleri—the MCED furthest along the path to widespread use—incorrectly flagged 57 healthy blood samples as cancerous in the aforementioned study.
There’s also a risk of jumping the gun—some cancers never become invasive or life-threatening, but early detection could prompt harsh treatment like chemotherapy. Some data suggests that less worrisome cancers actually show up in the bloodstream less, which could minimize that problem.
The NIC trial will help determine how blood test results for cancer should be interpreted, and it should provide a standard approach to launching cancer screening studies as companies flood the field with new tests.
“I don't think most companies tend to want to compare their tests head to head,” says Timothy Rebbeck, a professor of cancer prevention at Harvard. “It's expensive and difficult. So somebody else, a neutral party like the NCI, needs to.”
Rebbeck thinks the blood tests the new trial will vet will prove most helpful in the cases of pancreatic, liver, and ovarian cancer, which kill often and have no other form of screening. Still, longer trials are needed to confirm whether the time bought by these blood tests saves lives.
But Rebbeck is optimistic about the Cancer Moonshot’s ultimate goal: “It seems very realistic to me to think that we could reduce death by half,” he says.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.