At first glance, there’s nothing remarkable about the uninspired, low-rise hospital on the west side of Milan, affectionately known as “Gnocchi.” But two floors up, on an isolated wing of the Don Carlo Gnocchi IRCCS Centro S. Maria Nascente, an uncommunicative man with a severe brain injury is hooked up to a technology suite that researchers here believe can tell them if he’s conscious.
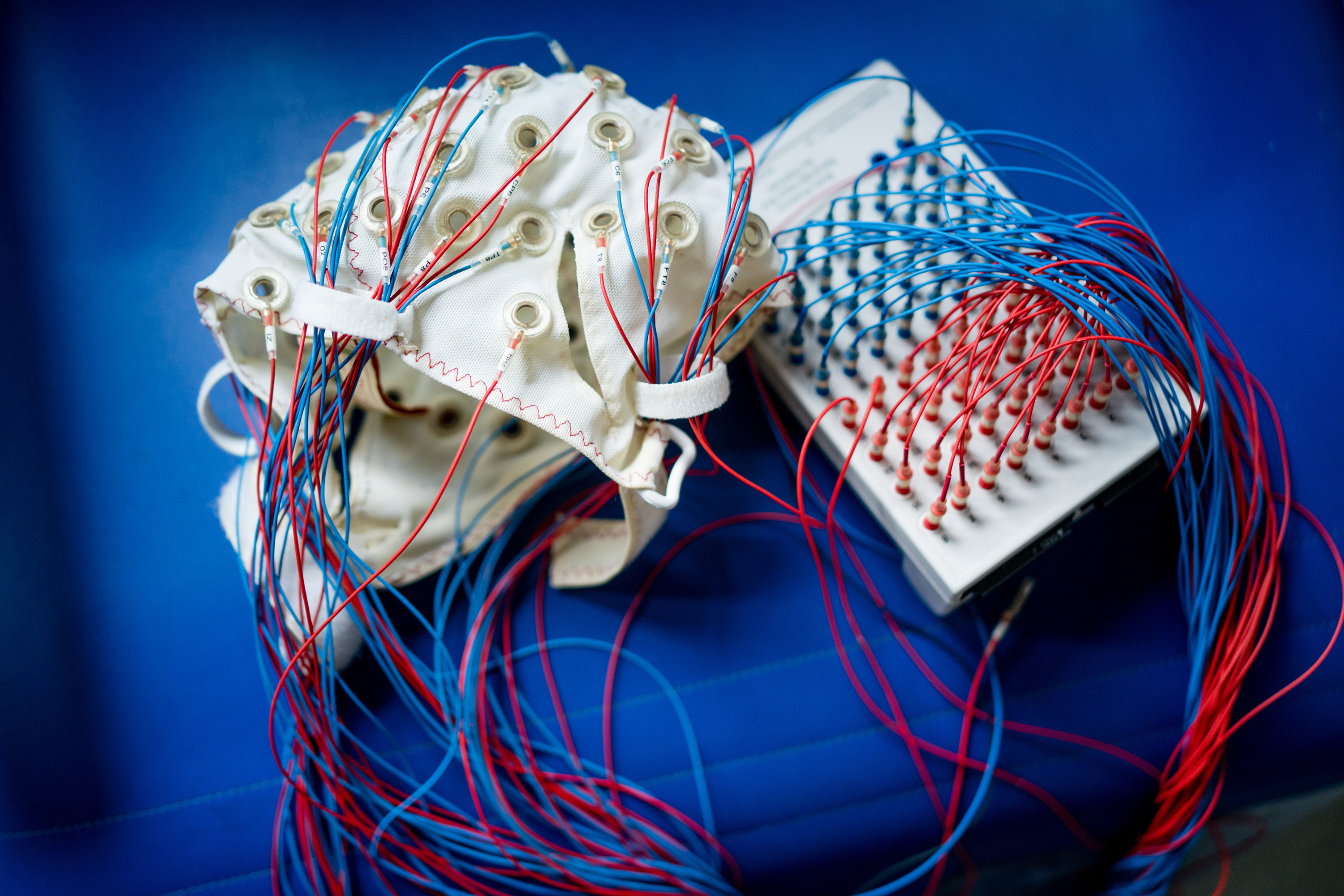
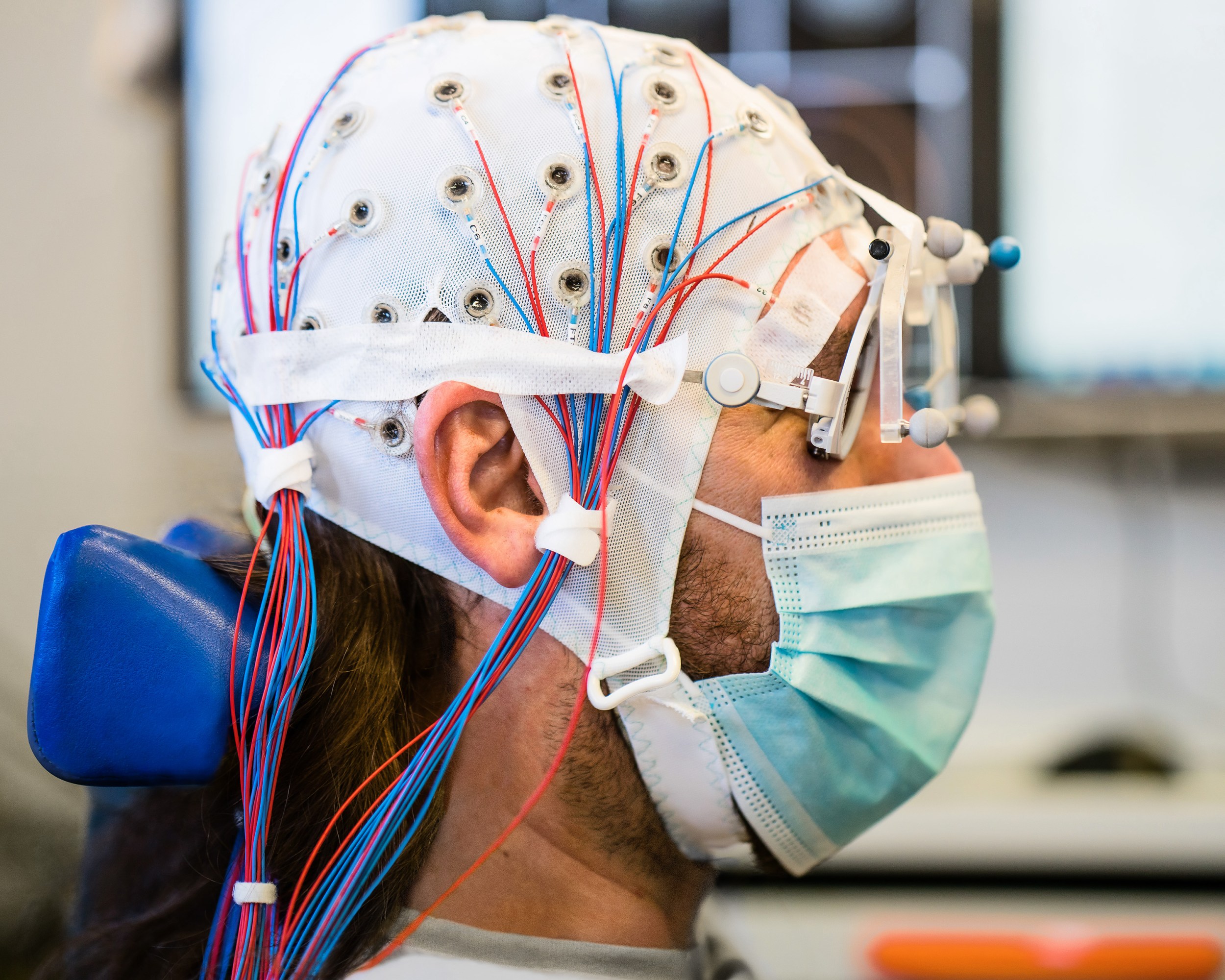
The man sits in what resembles a motorized dentist’s chair, his head cocked backwards, a blue surgical mask covering his mouth and nose. A white mesh cap dotted with 60 electrodes, each connected to a two-meter-long cable, is held in place by a strap beneath his chin. Hovering above him, an infrared array positioned on an articulating arm bounces signals off sensors attached to the man’s temples to produce a moving, MRI-constructed overlay of his brain on a nearby monitor. A researcher watching the monitor then presses a white plastic oval to the man’s skull and aims electromagnetic pulses at Tic Tac–size areas of his brain.
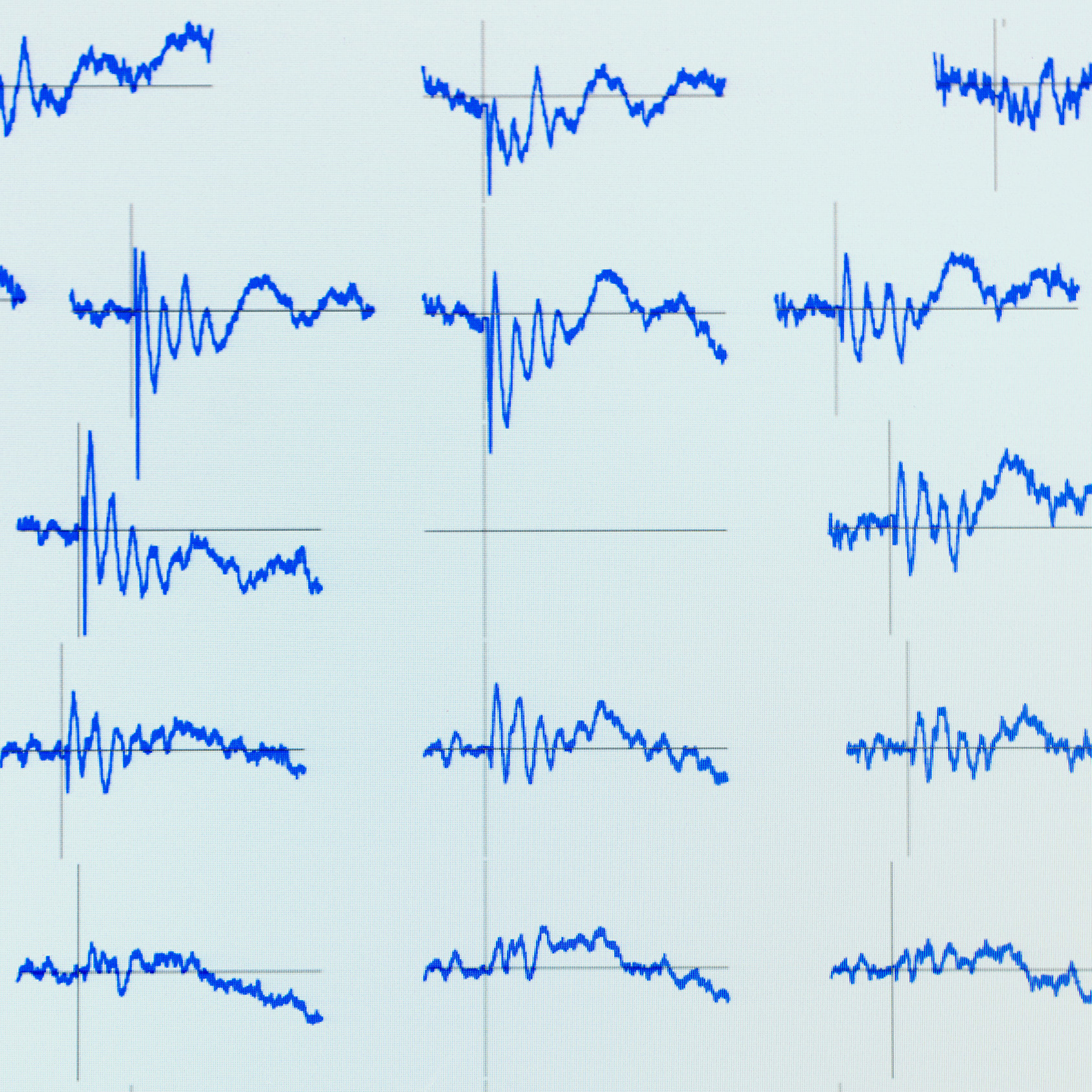
Each pulse makes an audible click. Three heavy cables, each about as thick as a garden hose, coil out from behind the device to a quarter-million-dollar machine controlling the output. On the other side of the room, Marcello Massimini, a blue-eyed, curly-haired neuroscientist, and Angela Comanducci, the patient’s neurologist, watch on a laptop as complicated blue squiggles representing brain waves fill the screen in close to real time. What the scientists see in them is the faintest sign of a liminal, maybe dreamlike, consciousness.
Back in the lab, a computer will assign those brain-wave recordings a number from 0 to 1—the so-called perturbational complexity index, or PCI. This single number, according to Massimini and his colleagues, is a crude measure of a type of complexity that reveals whether a person is conscious. The researchers have even calculated a cutoff of 0.31, which, according to a 2016 study of the technology in healthy and brain-injured subjects, “discriminated between unconscious and conscious conditions with 100% sensitivity and 100% specificity.” In other words, it works well—really well.
More unsettling is that when the researchers calculated PCI from a group of patients with unresponsive wakefulness syndrome (UWS, a condition previously known as a “vegetative state”), they found that around one in five had a PCI value within the consciousness distribution. “Even if [such a] patient is completely unresponsive, no sign whatsoever of consciousness,” Massimini told me, “you can say with confidence that this patient is nonetheless conscious.”
Such a breakthrough represents the most accurate consciousness meter ever seen in medicine (even if it is still crude, rudimentary, and unrefined). The medical implications are wide reaching. Estimates suggest there are up to 390,000 people around the world with prolonged disorders of consciousness. Some of them, unresponsive, may be treated as though nobody is in there—while they experience the world awake, alone, and unable to reach out from their bodily prison as long as they live.
Massimini is confident that PCI can help identify those people.
In July 2021, when I visited him in Milan, Massimini was collaborating with other researchers in Milan, Boston, Los Angeles, and beyond. In the meantime, PCI measurements are already being used at Gnocchi to help guide diagnosis and determine the potential for partial recovery.
The solution
PCI was born of the search to overcome nearly a century of obstacles standing in the way of measuring consciousness. Since 1924, when Hans Berger invented electroencephalography (EEG), scientists have tried to access the electrical responses that our brains use to communicate, hoping to see, predict, and measure what is going on behind the 6.5-millimeter-thick protection of our skulls. Berger’s invention detected changes in spikes of voltage produced by our neurons—converting those signals into the seismograph-like squiggles popularized as “brain waves.”
Standard EEG patterns include fast alpha waves, oscillating about 10 times a second and common in consciousness, and slow delta waves, oscillating about once per second and common in nondreaming sleep or under anesthesia. But passively listening to the brain with EEG is an imperfect way to determine consciousness, because exceptions are lurking everywhere.
The anesthetic ketamine can excite the brain, resulting in alternating alpha and delta waves. Some types of coma patients show fast oscillations while unconscious. And people under the influence of the drug atropine or during a seizure pattern called status epilepticus report being conscious while displaying the slow brain waves typical of unconsciousness.
An even bigger issue is that a patient’s brain activity itself—the result of short attention span, drowsiness, voluntary or involuntary movement, visual distractions, or even a lack of desire to follow instructions—can cause passive EEG to skew and react in ways that render its messages a mess.
The case for PCI is that it claims to be an objective measure of consciousness—a relatively straightforward yes or no. What differentiates it from regular EEG, according to Massimini, is that while the older technology only measures ongoing brain activity, PCI measures the brain’s capacity to sustain complex internal interactions. You can do this, he says, if you give the brain a knock and then follow how that perturbation filters and reverberates and is acted on as it courses through the fantastically complex architecture of 86 billion neurons and their 100 trillion connections in the human brain.
That knock or zap is delivered via trans-cranial magnetic stimulation (TMS), which has been around in modern form since the 1980s: a wand is held up against the head to shoot an electromagnetic impulse into the brain. When it’s used to target the motor cortex, TMS can provoke involuntary twitching of the hand; when it targets the visual cortex, it can induce lightning-like visuals in the mind’s eye.
To generate a PCI reading, Massimini uses TMS on the cerebral cortex. Then he uses EEG to measure what happens. It is the quality of the post-zap signal that leads to a score.

What Massimini looks for in this perturbed EEG is a special kind of complexity that is organized, but not too organized. The conscious mind produces neither the perfectly synchronized ripples of a stone lobbed into an imaginary pond nor the perfectly scrambled noise of an analog TV’s between-channel snow. The template of consciousness is more like an intricate chaos—a unique pattern among an almost infinite number of possibilities, with brain waves appearing similar in some areas and profoundly different in others.
Onscreen in the hospital, a high PCI looks like a series of squiggles that start off alike yet differentiate from one another as they move across the geography of the brain. A low PCI is even easier to see: either you get the same long, slow wave everywhere, or you get a wave in one part of the brain and silence everywhere else.
For years, Massimini and others could literally watch consciousness being recorded onscreen yet were stumped by how to quantify it.
They had clues for how to proceed, since the search for PCI was built on the foundation of integrated information theory (IIT), a controversial model of consciousness proposed by Giulio Tononi, a professor of psychiatry at the University of Wisconsin School of Medicine (see page 82). IIT claims that a conscious brain has a high level of integration (its various parts influence one another) alongside a high level of differentiation (the parts produce diverse signals).
Massimini was trying to find a proxy for this complexity that could actually be calculated in the lab, but the goal was elusive.
The “lucky strike,” as he recalls it, came from a bored Brazilian physicist named Adenauer Casali whose wife worked down the hall. Massimini offered Casali space in his office, where the physicist passed the time reading Dante and other Italian greats. One day the two started talking, and Massimini mentioned the problem.
“He’s in my lab, sitting on the chair,” recalls Massimini. “We start talking: ‘We’re doing this and that, and we have this problem, by the way—maybe you can add something?’” Indeed, the solution was obvious to Casali. All Massimini needed to do was take the TMS-EEG recordings and compress the data using the same algorithm a computer uses to compress files to the ZIP format. A low-complexity signal would end up being tiny because it would contain so little unique data. A high-complexity signal indicating a conscious mind would be large. Casali was credited as a first author on the paper introducing the quantification of PCI, and the procedure itself remains known as zap-ZIP.
Doubters
It’s a difficult thing to pursue something like PCI when experts still can’t agree on what consciousness is and isn’t. Tononi, who at times sounds like a mystic, explained the nature of consciousness to me with an example from everyday life. “You are lying in bed and asleep, a dreamless sleep, and then you wake up and suddenly there is something rather than nothing,” he told me. “That something is consciousness—having an experience.”
For most of history, detecting that something wasn’t all that difficult. If you asked someone a question and got a reasonable answer, that person was probably conscious.
“That’s still the gold standard,” says Massimini.
“[Massimini has] shown empirically that when the brain networks are shut down by anesthesia or sleep or brain injury, you have complexity patterns that are different from those seen when someone is awake.”
Emery Brown
But the increasing use of mechanical ventilation in the 1950s and 1960s helped create a significant populations of people with long-term disorders of consciousness for the first time. Today there are those who can be kept alive even though we have zero evidence of anyone being in there. And there are those like the gray-haired man at Gnocchi who show potential hints of consciousness, like eyes that track movement, but have no behavioral way to communicate or to prove their internal existence. Beyond is a whole spectrum of difficult-to-distinguish states. Tononi’s something is a condition we can all immediately identify in ourselves yet find difficult to know about in other people unless they tell us.
That makes any measure of consciousness controversial, let alone one whose theoretical foundation is IIT. While some scientists have called IIT the best theory of consciousness put forward to date, not everyone is a fan. When I wrote Michael Graziano, a neuroscientist at Princeton, about his opinion on IIT and PCI, his response was unequivocal.
“IIT is pseudoscience,” he wrote.
But, he continued, even phrenology—the idea, now firmly established as nonsense, that the shape of people’s heads can tell you about their personality—helped push science in the 1800s toward the idea that different parts of the brain had different functions, and that the cerebral cortex was worth some attention. “That change in perspective led to most of the major discoveries in brain science for a century,” he acknowledged, so PCI might still be worth something.
Emery Brown, a neuroscientist and anesthesiologist who is the director of the Harvard-MIT Program in Health Science and Technology, is reserving judgment, waiting for more evidence to come in. He’s wary of letting the “theory drive the analysis.” Yet Brown admires Massimini for doing experiments, carefully analyzing data, and publishing results for anyone to see.
“What I like about it, when I hear Marcello talk about it, is that he is being a total empiricist,” Brown told me. “He’s shown empirically that when the brain networks are shut down by anesthesia or sleep or brain injury, you have complexity patterns that are different from those seen when someone is awake.”
And that empiricism makes a compelling case when PCI values are computed in actual human beings.
Beautiful consistency
The power of Massimini’s approach is perhaps best represented in a beautifully consistent chart from years of testing the technology.
On the chart, PCI values computed from people known to have been conscious or not are recorded as dots separated by a dashed line at the threshold of 0.31. In every single case, the maximum PCI scores recorded in nondreaming sleep, or under the influence of one of three different anesthetic drugs, are below the line. And for the same people, every single one of the maximum scores while awake, experiencing the dreaming sleep of REM, or under the influence of ketamine (which at anesthetic doses induces a dreamlike state) is above the line.
So are nearly all the maximum scores for patients with locked-in syndrome and who had experienced strokes, who at the time of the study were able to prove their consciousness by communicating. Notably, 36 out of 38 patients in a minimally conscious state showed high complexity, demonstrating the unprecedented sensitivity of PCI as an objective marker of consciousness.
But nine of 43 patients previously considered totally without consciousness also scored above the line. This raises difficult questions. With no other way to prove their consciousness, and no way to communicate, those patients represent either PCI’s failure or its horrifying promise. Their zap-ZIP responses were similar in quality to those of people with minimal consciousness, as well as conscious people when awake, dreaming, or dosed with ketamine. And in fact, half a year after testing, six of these patients improved to the point that they were classified as minimally conscious. Someone, it seems, was in there after all.
In recent years, researchers in Massimini’s group have had the opportunity to stimulate neurons and record brain activity from electrodes temporarily inserted into the brains of patients having surgery for epilepsy. These measurements revealed an interesting mechanism by which PCI may collapse after brain injury, leading to loss of consciousness. Neuronal circuits that are physically spared by the lesion may enter a sleep-like mode, leaving the whole brain unable to generate complex patterns of interactions.
“Such intrusion of sleep-like neuronal activity may be only temporary in some patients, who will eventually regain consciousness, but may persist in others who remain blocked in a state of low complexity, corresponding to a prolonged vegetative state,” says Massimini. And that, he thinks, could provide a rationale for developing novel treatments to reawaken brain circuits and restore consciousness.
PCI could be refined in the form of other ways to perturb the brain, such as focused ultrasound or targeted laser light. Or the technology could be improved through better spatial-temporal resolution, or even automated scanning and computational calculations of where complexity is maximized in a damaged brain.
Massimini is clear that in its current form, PCI can’t say much about the quality or degree of consciousness—just whether it is there or not. And he sees the 0.31 threshold as a clinical measure of a blurry condition—it’s not the case that at 0.30 there’s nothing at all and at 0.32 consciousness appears in full form. You can have a high PCI score, he says, “and it doesn’t even make a difference whether you’re dreaming or awake.” Obviously part of the picture is missing.
Breaking through
But Angela Comanducci, a clinical neurophysiologist who passed through Massimini’s lab during her training and now oversees the 13-bed wing at Gnocchi that’s devoted to disorders of consciousness, has already observed the clinical power of PCI firsthand. In June 2020, a 21-year-old woman was brought to the ward two months after sustaining a traumatic brain injury from being beaten. “Every clinical diagnostic test, experimental and established, showed no signs of consciousness,” Comanducci told me. The situation was so dire that the family of the patient had been told to expect she would remain in an irreversible vegetative state.
But when Comanducci and her staff hooked the woman up to the bulky TMS-EEG apparatus used to measure her PCI, they were startled by what they saw. “Within seconds, I could see on the screen she was in there,” said Comanducci. The PCI they calculated later that day was high—reflecting high-complexity EEG response to TMS stimulation—and compatible with a minimally conscious state.
Over the next weeks they manually moved the patient’s fingers, arms, and legs, trying to reboot her brain the way you might start an old airplane by spinning its propeller. They spoke to her as if she was listening, trying to trigger a response—a sigh, perhaps, or the tiniest vertical movement of her eyes. And they administered a drug called amantadine, hoping to awaken parts of the brain they suspected might be undamaged yet in a state something like a protective sleep.
“I told my rehabilitation staff, ‘Now you must be detectives,’” recalled Comanducci. “‘Search everywhere and find her!’”
About a month later, they found her.
With a millimeter wiggle of a single finger, the woman opened a fragile portal of communication to the world outside. With practice, she learned to move more fingers, carving out a system with which she could answer simple questions.
Russ Juskalian is a freelance writer and photographer whose work has appeared in Discover, Smithsonian, and the New York Times.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.