The quest to learn if our brain’s mutations affect mental health
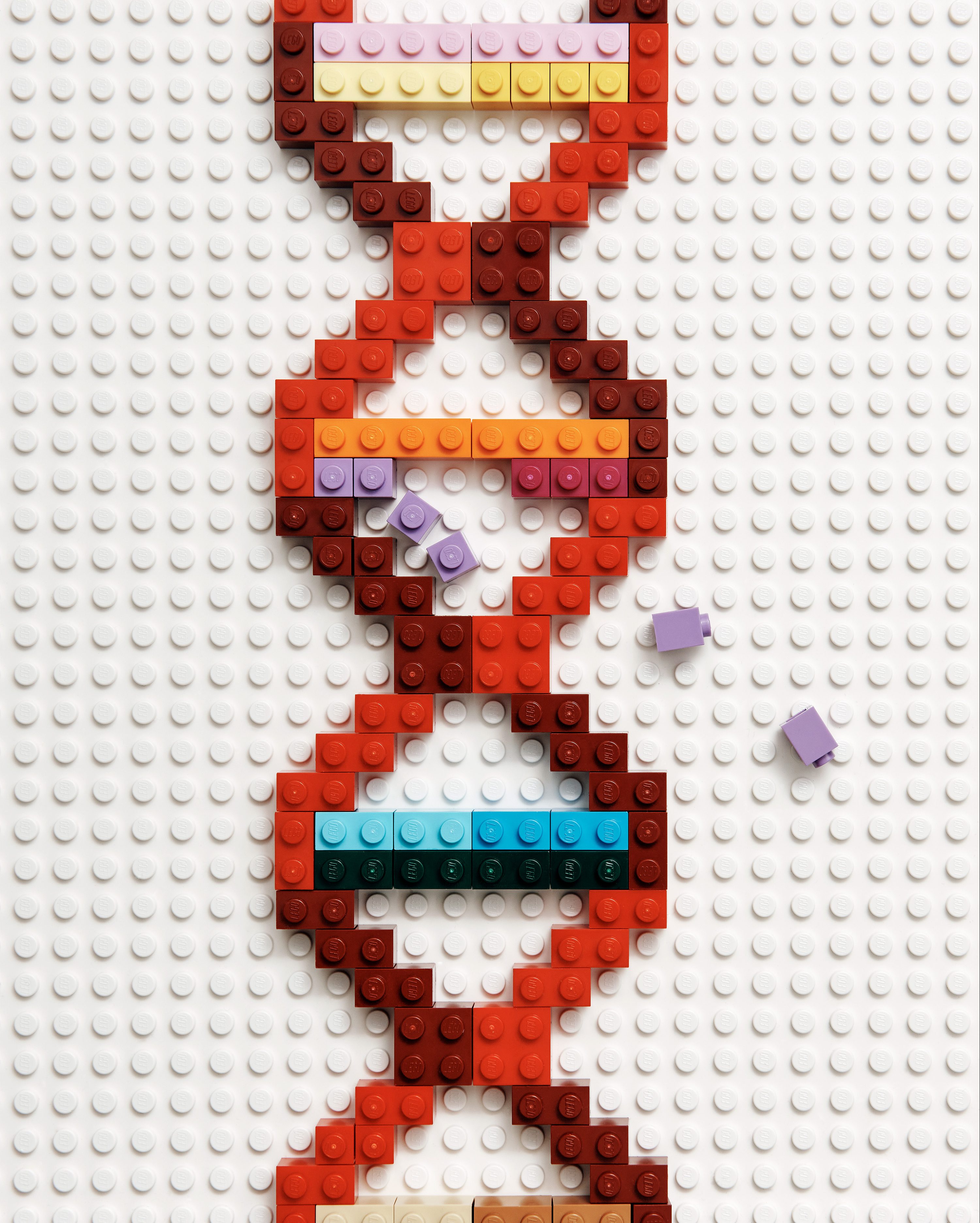
For years scientists have tried to find a gene for conditions like schizophrenia, Alzheimer’s and autism. But the real source could lie in a much more complex genetic puzzle.
When Mike McConnell decided what he wanted to spend his career working on, he was 29, inspired to begin his PhD—and flat broke. He’d learned from his biology classes that immune cells in the body constantly rearrange their own DNA: it’s what allows them to protect us by making receptors in the right shapes to bind to invasive pathogens. As he wrapped up a master’s degree in immunology in Virginia in the late 1990s, he’d obsess about it over beers with his roommates. “Suddenly this idea kind of clicked,” McConnell recalls. If gene rearrangement helped the immune system function, where else could it happen? What about the brain? “Wouldn’t it be neat if neurons did something like that too?” he thought.
At the time, most scientists assumed that cells in the normal nervous system had identical genomes. But McConnell looked through the scientific literature and found he wasn’t the only one hot on the trail of this question: a neuroscientist named Jerold Chun at the University of California, San Diego, was already working on it. He wrote to Chun and persuaded him to let him join his lab on the West Coast. There was just one problem: McConnell couldn’t afford to get there.
He was “a starving graduate student already,” with no cash to fix his navy 1966 Mustang—and as the first person in his family to go to college, he didn’t have access to many resources. “I didn’t have anybody who was going to drop some moving expenses in my lap or any of those sorts of things,” he explains. Chun gave him $1,000 to repair the broken car and get himself across the country so that he could start testing his hypothesis.
Using special dyes to stain the chromosomes of neurons from mouse embryos and adult mice, McConnell hoped to find that the neurons had undergone the same type of genetic rearrangement seen in immune cells, yielding diversity rather than the perfect copies most researchers would have expected. Instead, though, he kept finding brain cells that had the wrong number of chromosomes.

This was a surprise. When cells divide, they replicate their DNA for their daughter cells. Sometimes copies of genes are accidentally added or lost, which—unlike the reshuffling within chromosomes that’s beneficial in the immune system—was thought to be a hugely damaging mistake. It didn’t make sense that neurons could survive such a giant change in their genetic material. But McConnell kept finding aberrant neurons with extra or missing chromosomes. Finally he had to reconsider scientific assumptions. “We took the crazy idea seriously,” he says. A postdoctoral fellow in the lab named Stevens Rehen had expertise in culturing the neurons for study, which made it possible to parse the data.
The UCSD team’s experiments, published in 2001, showed that the central nervous systems of developing mouse embryos did not contain perfect genetic copies. Instead, the researchers suggested, about a third of the neurons from each mouse embryo, on average, had lost a chromosome or gained an extra one. The result was what’s known as a “genetic mosaic.” While many of those cells didn’t survive, some made it into the brains of adult mice. McConnell, Chun, and their coauthors wondered what such a genetic mosaic might mean. Perhaps in humans it could be a contributing factor to neurological disorders, or even psychiatric disease. In any case, it was an early clue that the conventional notion of genetically identical brain cells was wrong.
At the time, scientists seeking to understand the biology of mental illness were mainly looking for genetic mutations that had occurred near the moment of conception and thus were reflected in all of a person’s cells. Tantalizing clues had emerged that a single gene might be responsible for certain conditions. In 1970, for example, a Scottish teen with erratic behavior was found to have a broken gene region—and it turned out that his relatives with mental illness showed the same anomaly. It took three decades to isolate the error, which researchers named DISC1 (for “disrupted-in-schizophrenia”). Despite some 1,000 published research papers, the question of whether DISC1—or any other single gene—is involved in schizophrenia remains much debated. A handful of other genes have also been scrutinized as possible culprits, and one study of the whole human genome pointed to more than 120 different places where mutations seemed to heighten the risk of the disease. But after this extensive search for a “schizophrenia gene,” no single gene or mutation studied so far seems to exert a big enough influence to be seen as a definitive cause—not even DISC1.
In fact, scientists have struggled in their search for specific genes behind most brain disorders, including autism and Alzheimer’s disease. Unlike problems with some other parts of our body, “the vast majority of brain disorder presentations are not linked to an identifiable gene,” says Chun, who is now at the Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California.
But the UCSD study suggested a different path. What if it wasn’t a single faulty gene—or even a series of genes—that always caused cognitive issues? What if it could be the genetic differences between cells?
The explanation had seemed far-fetched, but more researchers have begun to take it seriously. Scientists already knew that the 85 billion to 100 billion neurons in your brain work to some extent in concert—but what they want to know is whether there is a risk when some of those cells might be singing a different genetic tune.
Ditching the dogma
McConnell, now 51, has now spent most of his career trying to answer this question. He seems laid back, at first, with his professorial short beard, square glasses, and slight surfer lilt. But there’s an intensity, too: he looks a little like a younger version of the Hollywood star Liam Neeson, with somber, spirited eyes and a furrowed brow. After earning his PhD, McConnell packed his bags once again and moved to Boston to start a postdoctoral position at Harvard Medical School. But he was restless. He didn’t relish the colder climate and longed to head back to California and revisit the data he’d found there on genetic differences in the brain. “I thought mosaicism was the most interesting thing I could be working on,” he recalls, sweeping the ends of his brown hair behind his ears, “and one Boston winter made me really miss San Diego.”
He started corresponding with Rusty Gage, a neuroscientist at the Salk Institute for Biological Studies in San Diego. Gage was also interested in genetic diversity, but he was best known for pushing against another piece of scientific dogma. People had long assumed that adults never made new neurons, but Gage had led a group that published a paper in the late 1990s detailing evidence of newly born cells in a brain region called the hippocampus.
The publication—establishing the evidence of what is called adult neurogenesis—gave him a reputation as a maverick who wasn’t afraid to stand behind provocative ideas.
Not too long after the UCSD team published its paper about mosaicism in the brain, Gage had struck upon another phenomenon that could explain how genetic diversity arises in the nervous system.
It was already known that cells had bits of DNA called long interspersed nuclear elements, or LINEs, which jump around the genome. Gage and his colleagues showed that these could also cause mosaics to emerge. In one experiment, mice engineered to carry human DNA elements known as LINE-1s developed genetically diverse cells in their brains as a result.
Just as with his work on neurogenesis, Gage initially encountered skepticism. The idea that LINEs—which many considered to be “junk” DNA—could cause genetic diversity in brain cells ran counter to the prevailing wisdom. “We knew we were going to run into a sawmill,” he recalls.
But Gage and his collaborators kept plowing ahead for more evidence. After the rodent study, he and his teammates looked at the human brain. Four years later, they published an analysis of postmortem samples, which found that LINE-1s seemed especially active in human brain tissues.
McConnell had been corresponding with Gage about all this, including the chromosome variation he’d found in mouse neurons while working in Chun’s lab. By the start of 2009, he’d secured a fellowship with Gage at the Salk Institute. There, they looked for evidence of the same phenomenon in human neurons, and after just a few years, they found it.
As part of the experiment, which appeared in Science in 2013, they used a new technology called single-cell genome sequencing. The technique could isolate and read out the DNA from individual cells; until then, scientists had only been able to analyze extracted genetic material from pooled cell samples.
Using the postmortem frontal cortex samples from three healthy individuals, they applied the method to dozens of neurons and established that up to 41% of the cells had either missing or extra gene copies. This variation was “abundant,” they concluded, and it contributed to the mosaic of genetic differences in the brain.
Instead of being genetically uniform, it turns out, our brains are rife with genetic changes. “We’re past the story about whether or not it occurs,” Gage says. “These mosaic events are occurring. This is very reminiscent of where I was with the adult neurogenesis. When everybody finally agreed that it occurred, we had to figure out what it did.”
Widening the search
After publishing data from human brains, McConnell didn’t feel he wanted to go back to studying mice. So when it came time for him to set up his own lab at the University of Virginia, he immediately set out to find human samples. “I spent the first three years as an assistant professor trying to find brains,” he recalls.
A couple of years after he landed in Virginia, the mission to understand the constellation of mutations in the brain got an important boost. The National Institute of Mental Health gave $30 million to a consortium including Gage, McConnell, and others so they could keep investigating somatic mosaicism. (“Somatic,” from the Greek for “body,” refers to mutations that arise during a person’s lifetime, rather than in the sperm or egg cells of the individual’s parents.)
The network contained research groups looking at the different effects of genetic mosaics. Gage and McConnell were part of a subset focused on the link with psychiatric disease. They devised a plan to look for different mechanisms for mosaicism using the same set of brain samples.
Crucially, they got human samples. Tissue biopsies of postmortem brains from individuals with schizophrenia were shipped from a repository in Baltimore, the Lieber Institute for Brain Development, to each of the three teams.
One portion of each was sent to Gage’s group in California to be examined for LINE-1s that might have caused mosaic genetic variation. Another portion was sent to McConnell’s team in Virginia to look for genetic mosaics caused by deleted or duplicated DNA in the genome.
The remaining third of each sample went to yet another lab, led by John Moran at the University of Michigan in Ann Arbor, which was investigating whether cells that acquire small DNA sequence errors very early in development might seed the formation of large brain regions with the same mutation.
There's a growing list of brain conditions where mosaicism really does seem to have a role. It has "reached proof for autism, epilepsy, and brain overgrowth disorders," says McConnell.
This January, a large group of scientists including members of the consortium published a paper in Nature Neurosciencedescribing how they used machine learning to analyze data about postmortem brain cells from several people who’d had schizophrenia. The researchers suggested that LINEs begin actively mutating brain DNA early in fetal development—and found instances where LINE-1s had bombarded at least two gene regions linked to neuropsychiatric disorders.
McConnell expects these kinds of discoveries to accelerate. He says that big improvements in genetic sequencing in the last few years now allow scientists to detect DNA errors at the individual cell level much more quickly. A couple of years ago it used to take four lab members on McConnell’s team two weeks to individually sequence 300 brain cells. Today, one team member working alone can do single-cell sequencing on 2,000 cells in three days. “It’s been a game-changer,” he says.
But finding mutations isn’t the same as establishing a causal link between them and disease.The sporadic and variable nature of mosaic mutations makes definitively connecting them to disease a complicated undertaking.Colleagues have cautioned him against chasing windmills in a quest that McConnell himself describes as “a little bit quixotic.”
Uncharted waters
The quest to understand how mosaic gene mutations might influence psychiatric disease stretches much further back than the work of scientists such as McConnell. He notes that decades ago “people were finding strange chromosome abnormalities in psychiatric diseases, largely in blood draws.”
But if you look to that history, you will see that those investigating the role of mosaic gene patterns in mental health have had false starts. One of the earliest case reports emerged decades ago: in the spring of 1959, a 19-year-old woman in southern England began stripping the paper off the walls of her newly decorated room. A month later, she burned all her clothes and ran away to the seaside town of Brighton. Her erratic behavior intensified to the point that she was admitted to a psychiatric hospital, where doctors diagnosed her with schizophrenia. They examined her blood and looked for the 46 wound-up bundles of chromosomes inside each cell. What they found surprised them: about a fifth of her cells were missing one of the two X chromosomes that women normally carry. The woman’s doctors were unsure whether her mosaicism was a factor in her psychiatric disorder. There are a handful of other cases of women who, like the British patient, were missing their second X in some cells and who also had schizophrenia. But the link remains pure speculation.
While it’s still too early to say how mosaic gene mutations in the brain might influence schizophrenia, there’s a growing list of brain conditions where mosaicism really does seem to have a role. For example, a pivotal 2012 study by Harvard geneticist Christopher Walsh and his colleagues uncovered evidence that somatic mutations were the root cause of some forms of epilepsy.
Perhaps the greatest amount of data on gene mosaics—and therefore the most promising area of development—is being generated from studies of autism. Various research groups, including Walsh’s, have found evidence that as many as 5% of children with autism spectrum disorder have potentially damaging mosaic mutation. More recently, in January, Walsh—along with consortium members like Rusty Gage—published a study uncovering evidence that certain types of mutations arise more commonly in people with autism. They looked at postmortem brain samples from 59 people with autism and 15 neurotypical individuals for comparison, and found that those in the first group had an unexpectedly high number of somatic mutations in the genetic regions called enhancers. These regions help stimulate the production of genes, which led the researchers to speculate that mosaic mutations there might elevate a person’s risk of developing autism.
And even though brain cells are not thought to be actively dividing like cells in other tissues, they do seem to develop into more of a genetic mosaic as we age. In 2018, the team led by Walsh analyzed neurons taken from the brains of 15 people four months to 82 years old, as well as nine people with disorders linked to premature aging. They concluded that the somatic changes in DNA that create a mosaic accumulate “slowly but inexorably with age in the normal human brain.” A new study from Walsh’s group, still undergoing peer review, suggests that while human neurons begin with hundreds of such mutations in every genome, mutations continue to build at a rate of up to 25 per year for life. On this basis, he and his teammates calculated that neurons in elderly individuals contain somewhere between 1,500 and 2,500 mutations per cell. “We think that this is a key new way of looking at aging and common forms of neurodegeneration like Alzheimer’s disease,” Walsh says.
British scientists looking specifically for somatic variants in genes associated with neurodegenerative disorders such as Parkinson’s and Alzheimer’s suggest that the average adult has 100,000 to 1 million brain cells with pathologically mutated genes. The next step is to understand whether and how those mutations actually exert an influence.
Identifying the link between mosaics in the brain and various medical conditions isn’t just about explaining how these illnesses arise, though.One of the greatest hopes is that it might help usher in new therapeutic approaches. That’s already happening with one condition, an often untreatable form of epilepsy known as focal cortical dysplasia. The brains of individuals with this disorder have telltale spots of disorganized tissue layers, and patients sometimes undergo surgery to remove these brain areas in the hope of reducing their seizures.
A study published in 2018 by researchers at the Korea Advanced Institute of Science and Technology found mosaic mutations in these abnormal brain spots that overstimulated certain cell-signaling pathways. Drugs that curb this overactivity, called mTOR inhibitors, are worth a shot, according to scientists.
“I think it’s largely uncharted waters,” says Orrin Devinsky, who is leading a pilot trial for a drug to treat focal cortical dysplasia at the New York University Langone Medical Center. “There’s a few areas where we’ve made real progress … but I think with the larger field the ground has barely been touched.”
On the brink
Twenty years after he started, Mike McConnell remains as fascinated as ever with the question of how genetic mutations acquired after conception or birth might shape our behavior. “My interest really became: What makes outliers?” he says, with the California tone that he brought back with him to the East Coast. “What makes two identical twins totally different people?”
In all that time, a lot has changed. He’s married and settled down, he’s earned awards from the likes of the US National Academy of Medicine, and he’s not a destitute grad student anymore. He recently switched coasts again, moving his lab to the Lieber Institute, which is home to more than 3,000 brains—one of the world’s largest collections.
And he thinks we’re on the brink of a breakthrough.
Even if the links between mutations and mental conditions are not conclusive, scientists in the field now feel they have amassed a trove of data to show that having genetically different cells can certainly influence our health. “Brain somatic mosaicism has reached proof for autism, epilepsy, and brain overgrowth disorders,” McConnell says.
The evidence, meanwhile, continues to accumulate that many people have significantly mosaic brains. One 2018 analysis suggests that around 1 out of every 100 people has deleterious mosaic genetic difference that affects “sizable brain regions.” In other words, they have a section of brain cells that possess a mutation not seen in surrounding cells. However, while there’s increasingly solid evidence that mosaic gene patterns in the brain contribute to epilepsy and autism, there isn’t enough data yet to implicate them in schizophrenia.
McConnell has kept the faith that studying human brains will reveal whether some “flavor” of mosaic mutations contributes to that disease too—mutations that could point toward new treatments. “I’m either going to have a eureka moment, or this is just something that happens and there’s not a clear link to disease,” he says. Ever the optimist, he hopes to succeed where others have failed by sorting through the flood of genetic data pouring in about the brain cells he’s analyzing. “If there’s a signal there,” he says, “I think I’m going to see a hint of it in the upcoming year.”
Roxanne Khamsi is a science journalist based in Montreal. This story was supported by a reporting grant through the Genetics and Human Agency Journalism Fellowship.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.