Taking the pandemic’s temperature
Inder Singh’s smart-thermometer startup provides real-time fever data to combat covid-19.

Last March, as covid-19 ripped through communities across the country, Inder Singh, MBA ’06, SM ’07, realized he had information that could help officials respond.
For years Singh’s company, Kinsa Health, had tracked fevers using data from its network of thousands of smartphone-connected thermometers. As the potential scope of the covid-19 outbreak became clear, Singh subtracted the typical cold and flu numbers gathered in years past from the company’s graphs.
“What’s left over are unusual fevers, and we saw hot spots across the country,” Singh says. “We observed six years of data and there’d been hot spots, but nothing like we were seeing in early March.”
Kinsa’s team realized that the data offered a more immediate view of illness than test results. Within days they made it publicly available. Then on Saturday, March 14, Singh got on a call with the former head of the US Food and Drug Administration, the physician-researcher responsible for Taiwan’s successful covid-19 response, and Nirav Shah, a physician who is the former New York state health commissioner.
“Inder showed us this map, and he said, ‘I think this is covid-19 in the community,’” recalls Shah, who serves as an advisor to Kinsa. “All three of us were like, ‘It’s lighting up in Texas and Florida—we don’t see any covid [hot spots] there. Obviously your stuff is wrong.’” Two weeks later, the first surges in cases started being reported out of Texas and Florida.
Since then, Kinsa has been working to help US efforts to understand and contain the virus. Its data is being used by officials in at least five states and five cities, thousands of research groups, prominent media outlets, and organizations including the NBA, which used Kinsa’s thermometers during the isolation of its players and coaches to finish the 2019-2020 season.
Kinsa’s FLUency Program, an initiative started in 2013 to help schools combat the seasonal flu, laid the foundation for Kinsa’s data collection. Today the company is working with more than 4,000 schools, accounting for about 5% of the nation’s public elementary schools.
“By the time the CDC [US Centers for Disease Control] gets the data, it has been processed, deidentified, and people have entered the health system to see a doctor,” says Singh, who is Kinsa’s CEO. “There’s a huge delay from when someone contracts an illness to when they see a doctor. The current health-care system only sees the latter; we see the former.”
Finding a path
Singh, who earned undergrad degrees in economics and engineering at the University of Michigan, was introduced to the world of infectious disease during graduate studies at the Harvard Kennedy School of Government. Although he’d started college intent on becoming an astronaut, as a grad student he spent time in different parts of Africa working on initiatives to prevent the spread of diseases like malaria and AIDS.
Singh’s first exposure to MIT came while he was back in Cambridge.
“I remember I interacted with some MIT undergrads. We brainstormed some social-impact ideas,” he recalls. “A week later I got an email from them saying they’d prototyped what we were talking about. I was like, ‘You prototyped what we talked about in a week?’ I was blown away, and it was an insight into how MIT is such a doer campus. It was so entrepreneurial.”
Soon Singh enrolled in the interdisciplinary Harvard-MIT Program in Health Sciences and Technology, earning his master’s and MBA degrees while working with leading research hospitals in the area. He then got what he describes as a dream job at the Clinton Health Access Initiative (CHAI), brokering deals between pharmaceutical companies and poor countries to lower the cost of medicines for AIDS, malaria, and tuberculosis. The role opened his eyes to several shortcomings in the global health system.
“The world tries to curb the spread of infectious illness with almost zero real-time information about when and where disease is spreading,” he says. “The question I posed to start Kinsa was ‘How do you stop the next outbreak before it becomes an epidemic if you don’t know where and when it’s starting and how fast it’s spreading?’”
Thermometers for change
With the insight that better data was needed to control infectious diseases, Singh founded Kinsa in 2012. In order to get that data, the company needed a new way of providing value to families when someone was ill.
“The behavior in the home when someone gets sick is to grab the thermometer,” Singh says. “We piggybacked off of that to create a communication channel to the sick, to help them get better faster.”
A year later, the company launched the FLUency Program, which became the vehicle for Kinsa to get millions of thermometers into communities around the country. The company relies on donations and government grants to hand out its thermometers to schools that serve primarily poor families.
Kinsa’s thermometers link to an app that considers age, temperature, and symptoms to help users decide if they should seek medical attention. The app also incorporates community illness levels into its guidance—informing parents, for instance, if other students in their child’s grade have come down with the flu.
“That’s important because parents question what’s going around,” Singh says. “For the most part everything starts the same way: a cough, maybe a spike in fever. But what is it? Strep throat? Common cold? Flu? Covid-19? Now you have more context.”
The data generated by the thermometers is also anonymized and aggregated for officials like school nurses, who can help prevent the spread of disease in classrooms by reminding parents to keep their kids home if they are sick or by encouraging teachers to disinfect surfaces more often.
In California, Fresno began equipping families in each of its 60 elementary schools with thermometers in 2019. Kinsa looked at the number of student absences in schools with more and less participation in the program and found that students missed 8% fewer days in schools where more families had thermometers, a pattern school officials also noticed.
“Students miss less school because we’re not exposing as many kids to illness,” says Jane Banks, the head of school nurses for the Fresno public schools. “We’re educating and intervening in real time when we see any outbreak, or anything that’s off.” In the fall, she was talking with Kinsa about how Fresno might use the thermometers to help bring students back to the classroom in phases once schools got the green light.
In Laguna Niguel, California, the Community Roots charter school distributed the thermometers to all students’ families after beginning the school year with online instruction. When the school shifted to in-person learning, it required students arriving on campus each day to show school officials their negative fever results through the Kinsa app. While of course being fever-free can’t guarantee that a student is covid-free, the daily temperature readings at home at least made it possible to keep symptomatic students away from healthy students. As of the beginning of December, Community Roots was the only elementary school open for five-day classroom instruction in Orange County.
“I interacted with some MIT undergrads. We brainstormed some social-impact ideas. A week later I got an email from them saying they’d prototyped what we were talking about. I was like, ‘You prototyped what we talked about in a week?’ I was blown away.”
Singh says the only thing holding the FLUency Program back is funding: an additional 13,000 schools have applied to participate, but Kinsa hasn’t found enough donors. “We are adamant that we don’t charge the public schools,” he says.
Kinsa’s fever data has proved useful beyond school settings as well. In the Orlando “bubble” the NBA used to finish its 2019-2020 season, every player, ref, media person, and staff member began each day with a reading from Kinsa’s thermometer. If someone showed a higher temperature than average, the NBA’s health and safety team, which included doctors and epidemiologists, would call the person to do an assessment. John DiFiori, the NBA’s director of sports medicine, told USA Today the daily temperature check was “really the foundation” of the league’s approach to keeping everyone safe.
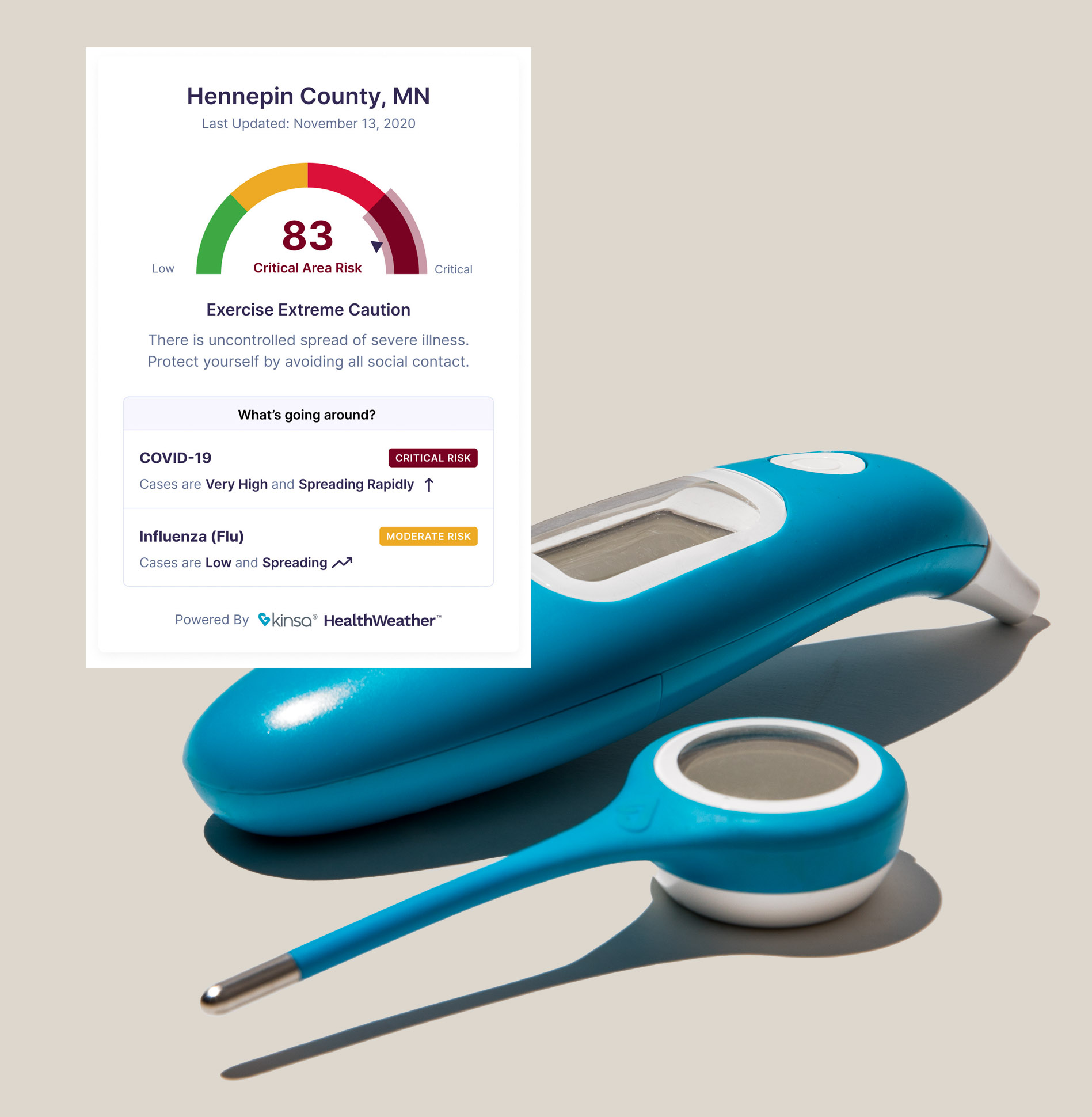
Kinsa has also made information about local outbreaks available to anyone—not just those with the app. In November, the company launched a tool on its HealthWeather website that lets anyone in the US view a real-time risk score for the level of contagious illness in a given zip code. The idea is to make checking local illness levels as easy as viewing local weather forecasts.
Fever data is not a perfect proxy for covid-19 infection. It can do only so much to help authorities contain the virus because people can be asymptomatic but still contagious, cautions Joseph Frassica, a professor of the practice at MIT’s Institute for Medical Engineering and Science (IMES) as well as the head of Philips Research North America. Younger populations are more likely to be asymptomatic if infected, he says, which particularly limits the usefulness of student testing systems that rely on temperature data alone.
That said, he thinks that combining fever data with the questionnaires on Kinsa’s app is a great way to track symptomatic covid-19 cases, and Kinsa’s widespread thermometer distribution means that its maps are a fairly good indicator of covid-19 in communities. Kinsa says that between March 1 and November 1 of 2020, it captured nearly 15 million fever readings and 1.7 million symptom inputs.
“Kinsa’s approach of collecting data from connected thermometers is an important one and actually very useful for detecting geographies where there’s an increase or decrease in the incidence of fever—and, in the year of covid-19, the incidence of covid-19,” says Frassica, who has worked on building predictive models for covid-19 through IMES and is not affiliated with Kinsa Health.
Filling a void
Last spring, New Orleans city officials were working overtime in a struggle that was playing out across the US. The city had organized a covid-19 response team to establish community testing sites, procure protective equipment, educate the public, and take other steps to curb the spread of the disease.
Unfortunately, like the rest of the country, New Orleans had to rely on testing data to track the virus. That made it more likely that people would spread the disease before they knew they were infected.
The mayor’s office had been in touch with Kinsa about the company’s thermometers, but the city was in no position to buy them anytime soon.
Then a Kinsa employee called the mayor’s office to say the company had found a donor, and 25,000 thermometers were coming free of charge. They arrived at city hall on June 24. Over the next few weeks, the thermometers were given out to low-income families, who are generally more vulnerable to the worst symptoms of covid-19. Many of the recipients didn’t previously have a thermometer in their home. Kinsa’s app gave the families information about the spread of the disease in their communities and helped them take steps to mitigate its spread. It also gave city officials new, real-time information about community health.
“If I know what’s going on in the community, I can respond better as a parent, I can respond better as a school leader, I can respond better as a school nurse,” Singh says. “When you know where and when symptoms are starting and how fast they’re spreading, you can empower local individuals, families, communities, and governments.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.