This stem-cell implant could halt an incredibly common cause of blindness
An eye implant made of a thin sheet of human embryonic stem cells might be an effective treatment for a common form of vision loss.
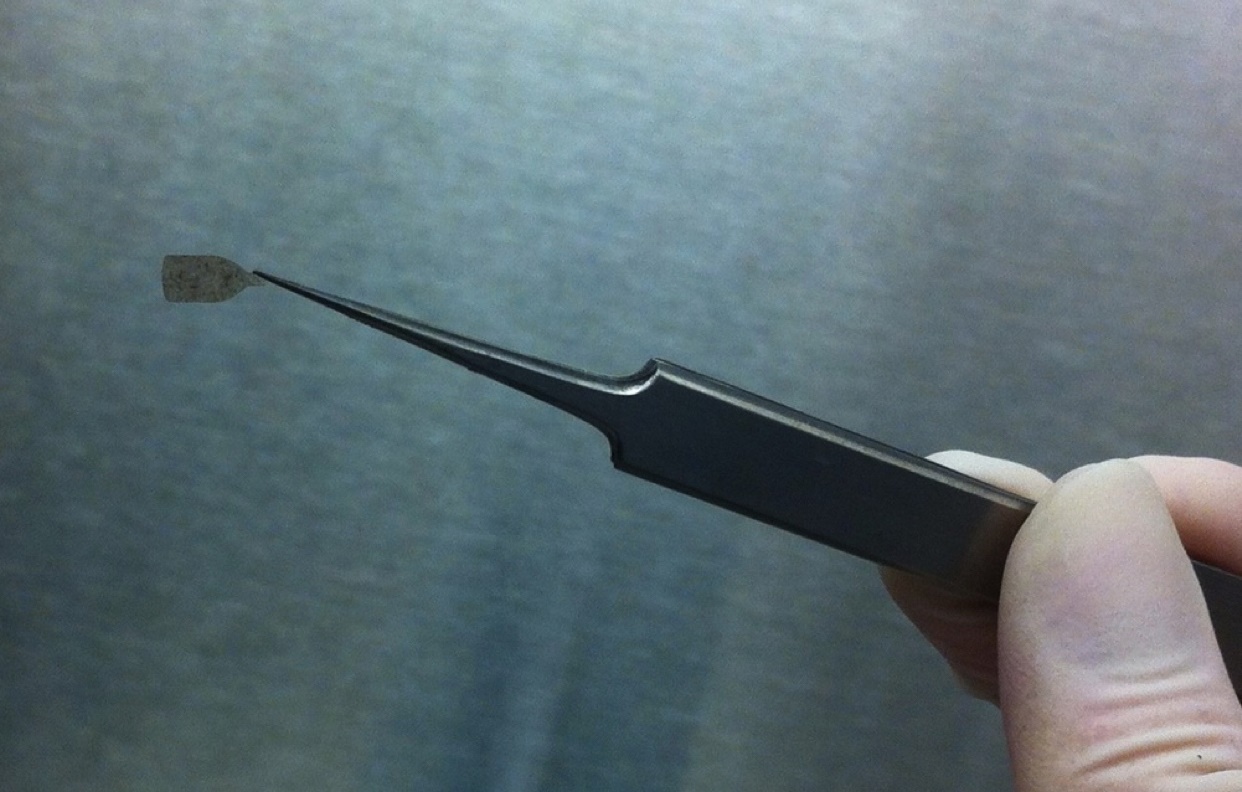
Researchers at the University of Southern California grew stem-cell membranes in a sterile lab for a month and then inserted them into the eyes of four people with “dry” macular degeneration, the leading cause of blindness in developed countries. An estimated 196 million people worldwide will have some form of macular degeneration by 2020.
People with the dry type suffer from a progressive thinning of the retinal pigment epithelium, a layer of cells that support and nourish the light-sensing photoreceptors. Without this vital layer, which the implant is intended to replace, the photoreceptor cells also die off, and people slowly lose their eyesight.
Researchers monitored the four patients over the course of a year, and found that their eyesight didn’t decline.
The study was meant to test the safety of the implant, so only patients with very advanced macular degeneration were included. Because of that, study author Amir Kashani says, he didn’t expect an improvement in vision. “But after surgery, one patient could read 17 more letters on an eye chart than before surgery,” he says.
Two patients were also able to focus their gaze better than before. The results appear today in the journal Science Translational Medicine. Kashani thinks the implant will be more effective for people in earlier stages of the disease.
When stem cells were first extracted from human embryos 20 years ago, scientists marveled at their ability to change into any type of cell in the body and thought they would soon be used to treat all types of diseases, from eye disorders to diabetes. But that dream has yet to be realized. There are no embryonic stem-cell treatments approved by the US Food and Drug Administration, and most human studies of such therapies have shown unremarkable results.
Researchers have, for example, tried injecting embryonic stem cells directly into the eye, but the cells moved around in the eye and weren’t very effective. “The reason we’re encouraged is that we’re replacing the exact anatomical defect that is causing the disease,” Kashani says.
Another research team, at Moorfields Eye Hospital in London, recently reported that a similar stem-cell patch they developed was able to restore sight in two patients with the wet form of macular degeneration, which is caused by abnormal blood vessels that leak into the central part of the retina.
But both studies were small and neither had control groups, so it’s hard to know whether the perceived benefits can actually be credited to the stem-cell therapies.
Paul Knoepfler, a stem-cell biologist at the University of California, Davis, says work on stem-cell therapies has been slow because of the tremendous safety risks involved. “We’ve seen what can go horribly wrong with shortcuts with stem cells by for-profit clinics,” he says.
Last year, for example, the FDA vowed to crack down on spurious clinics that blinded patients with eye injections of stem cells derived from people’s fat.
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.