Nanoparticle Detects the Deadliest Cancer Cells in Blood
Patients and doctors often don’t know if surgery to remove cancerous tissue was successful until scans are performed months later. A new kind of nanoparticle could show patients if they’re in the clear much earlier.
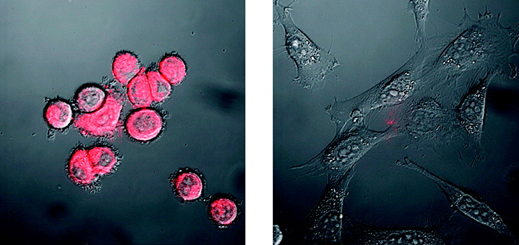
The nanoparticles—dubbed nanoflares—attach themselves to individual cancer cells in a blood sample and then glow, allowing cancerous cells to be detected and sorted with the help of a laser. Since different types of cancer cells—some of which are far more lethal than others—can be detected and collected using the technique, and since those cells can then be cultured in a dish, the nanoparticles may also make it easier to test potential treatments before giving them to patients.
In a paper published in the journal Proceedings of the National Academy of Sciences, researchers show that the nanoparticles can detect different types of breast cancer cells in mice. They also show that they could identify breast cancer cells added to human blood in a lab. The next step is to see whether the particles can find cancer cells in blood samples from patients.
Each nanoflare consists of a chunk of gold coated with fluorescent molecules and snippets of DNA. The DNA is selected to correspond to RNA found in particular cancer cells. Once introduced into a blood sample, the nanoparticles will enter cancer cells and the DNA will bind to the target RNA, triggering the release of fluorescent molecules and causing the cancer cells to glow. Different types of cancer cells can be detected by attaching different strands of DNA and fluorescent molecules of different colors.
Circulating tumor cells are “the most lethal kind,” because they allow cancer to spread, says Melissa Skala, a professor of biomedical engineering at Vanderbilt University. Such cells, however, are challenging to find because they occur in such small numbers.
Other researchers are developing similar approaches for detecting circulating tumor cells, often using nanoparticles that bind to the surface of cancer cells. The new approach offers two potential advantages, says Shad Thaxton, a professor of urology at Northwestern, and one of the researchers involved in the work. As well as making it possible to better differentiate between various cancer cells, the approach keeps cells alive so they can be cultured, while other approaches tend to destroy them.
It may take years for nanoflare-based tests to be approved for treating breast cancer or other forms of the disease. But even before then, nanoflares could be used to better understand cancers and help discover new drugs, says study author Chad Mirkin, director of the International Institute for Nanotechnology at Northwestern University. That’s because the technique allows specific types of cancer to be cultured and tested in the lab, he says.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.