A Laboratory for Rare Cells Sheds Light on Cancer
In 1869, the Australian physician Thomas Ashworth put the blood of woman who had died of breast cancer under a microscope. Peering through it, he spotted “cells identical with those of the cancer itself.”
He postulated that the large and abnormal cells in her blood might explain metastases all over her body, more than 30 of them. The cancer cells were probably moving through the circulatory system, creating the rash of tumors.
In a new report published in Science, researchers at Massachusetts General Hospital say that after capturing these “circulating tumor cells” from patients fighting cancer, they have been able to keep them growing in the lab, and tested drugs against them.
The work is a “critically important proof of concept study” that shows how researchers might one day undertake personalized studies on patients’ own tumor cells, says Stefanie Jeffrey, a cancer expert at Stanford University.
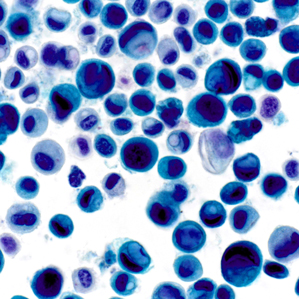
The circulating tumor cells are extremely rare—they account for one of every billion cells found in a patient’s blood. Yet the researchers were able to pluck tumor cells from the blood of six patients with advanced breast cancer and then culture them, or keep them alive and multiplying. While scientists at Baylor University first showed last year that culturing tumor cells from the blood was possible, the Boston scientists also managed to place the cells into micro-vessels—each holding about 200 cells—and test whether they could be killed with one or more drug treatments.
Daniel Haber, the Mass. General oncologist who led the study, says the approach could eventually help resolve common situations he faces in his clinic, when patients stop responding to an initial treatment. Which drug to give them next is often little better than a guess. “You need to know what you are treating,” says Haber.
Over the last decade, a huge amount of effort has gone into engineering devices able to capture cancer cells in the blood, including technologies like “nano Velcro,” magnetic sifters, and simple paper filters. The Mass. General device, called the CTC-iChip, was created over the last three years in the lab of engineer Mehmet Toner and is considered one of the most advanced (see “Device Finds Stray Cancer Cells in Patients’ Blood”).
At Toner’s lab, vials of blood set into the instrument rock back and forth, dripping fluid through a series of microchannels that remove normal blood cells. After about half an hour, all that’s left is a plastic bag filled with a small number of the rare cancer cells. Development of the device has been paid for by Johnson & Johnson, which has spent $30 million funding the work.
Johnson and Johnson already sells a system called Cellsearch that can count tumor cells in the blood. But that device, approved by the FDA in 2004, has not proved so useful to doctors. The number of tumor cells in someone’s blood predicts their chance of surviving, but it doesn’t help doctors know how to treat the patient.
Some doctors aren’t sure that personalized testing of tumor cells will help either. One problem is that it’s very difficult, and took the Mass General team months of effort to grow cells from the patients. That’s too long to be helpful in picking a treatment; some patients don’t survive that long. “It’s expensive and it takes several months. I don’t think this is going to have a future for patient care,” says Massimo Cristofanilli, an oncology specialist at Jefferson University Hospital, in Philadelphia.
Stanford’s Jeffrey adds that it’s still unclear whether cancer cells in the blood are really the same as those in a person’s tumors. That means it’s uncertain if tumors and the cells will respond in the same way to drug treatments.
Instead, the technology may prove more important in studying how metastases occur. As Ashworth hypothesized in the 19th century, cancer cells must spread through the bloodstream. Yet very little is known about what makes a cell metastatic and able to escape into the blood and take hold elsewhere.
“These are very rare cells that circulate for a very short time and disappear,” says Haber. Yet they “may be responsible for the vast majority of cancer deaths. This is a technology that lets you look at something you could never see before.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.