Closing a Back Door for Cancer
About half of all cancer patients have a mutation in a gene called p53, which codes for a tumor-suppressing protein that controls cell division. That mutation allows tumors to continue growing even after chemotherapy damages their DNA.
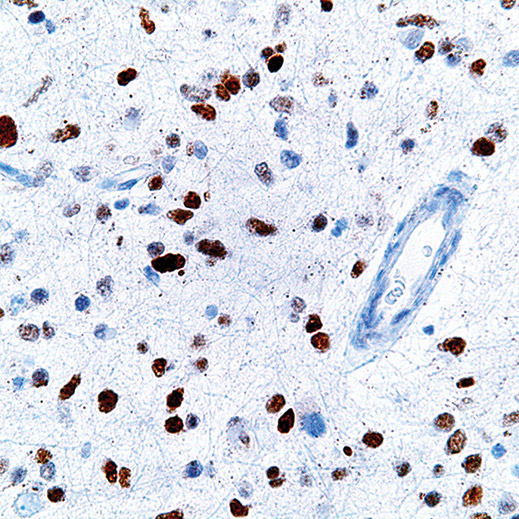
A new study from MIT biologists has found that tumor cells with mutated p53 can be made much more vulnerable to chemotherapy by blocking another gene, called MK2. In a study of mice, tumors lacking both p53 and MK2 shrank dramatically when treated with the drug cisplatin, while tumors with functional MK2 kept growing.
The new findings suggest that giving cancer patients a combination of a DNA-damaging drug and an MK2 inhibitor could be very effective, says biology professor Michael Yaffe, senior author of a Cell Reports paper describing the research. He notes that while several drugs that inhibit MK2 are now in clinical trials to treat inflammatory diseases such as arthritis and colitis, they have never been tested as possible cancer treatments.
Before cell division begins, p53 checks the cell’s DNA and initiates repair, if necessary. If DNA damage is too extensive, p53 forces the cell to undergo programmed cell death, or apoptosis. Tumors that lack p53 can avoid this fate.
“Usually p53 is the main driver of cell death, and if cells lose this pathway they become very resistant to different treatments,” says Koch Institute postdoc Sandra Morandell, who was lead author of the paper.
Yaffe’s lab had previously discovered that the MK2 gene helps counteract the effects of chemotherapy in cancer cells with mutated p53. When the drugs damage cancer cells’ DNA, MK2 puts the brakes on the cell division cycle, giving them time to repair the damage before dividing. “Our data suggested if you block the MK2 pathway, tumor cells wouldn’t recognize that they had DNA damage and they would keep trying to divide despite having DNA damage, and they would end up committing suicide,” Yaffe says.
In the new study, the researchers used a strain of mice that are genetically programmed to develop non-small-cell lung tumors. They further engineered the mice so that the MK2 gene could be turned on or off. That way, tumors with and without MK2 could be studied in the same animal.
Before treatment, tumors lacking both MK2 and p53 grew faster than tumors with MK2. This suggests that treating tumors with an MK2 inhibitor alone would do more harm than good, possibly increasing the growth rate by taking the brakes off the cell cycle. But cisplatin shrank the tumors lacking MK2 without affecting the others.
The researchers have found similar results with cancer cells grown in the lab from bone, cervical, and ovarian tumors. They are now studying mouse models of colon and ovarian cancer.
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.