Finding Cancer Cells in the Blood
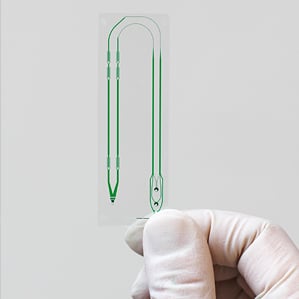
In the near future, oncologists may be using a finger-size plastic chip with tiny channels to extract a dozen or so cancer cells from a sample of a patient’s blood. Those cells, called circulating tumor cells, could then be screened for genetic disruptions that an oncologist could target with drugs best suited to attacking the tumor. Continued sampling would give doctors a way to monitor whether a treatment is working and decide whether to add or change a drug as the malady evolves.
Dozens of companies are vying for success in this market, which is expected to reach $7.9 billion in the next few years, but so far only one device, sold by a Johnson & Johnson subsidiary, has received FDA approval. That current technology is not able to detect circulating tumor cells when they’re present only in very small numbers, says Daniel Haber, director of the Massachusetts General Hospital Cancer Center, and cannot capture the full diversity of cells that escape from different tumor types in patients. But advances are already proven in labs and may be making their way to clinics in the next few years, experts say.
Working with biomedical engineer Mehmet Toner and his team at MGH, Haber is developing their latest chip into a commercial product. The new chip design can pull out any cancer cell that might be floating in the blood and keep it alive so pathologists can do genomic and molecular tests on it (see “Device Finds Stray Cancer Cells in Patients’ Blood”). The results of such tests are valuable because pharmaceutical companies are increasingly developing cancer drugs with specific molecular targets in mind. These targeted therapies stand to improve cancer treatment. Cancer genomics company Foundation Medicine says that as many as 70 percent of tumors it analyzes carry genetic signatures that can inform treatment (see “Cancer Genomics”).
Although the scientific and medical community has long known that cancer spreads through the bloodstream, there has been no way to capture the circulating tumor cells. “These are rare cells in the midst of 100 billion other cells,” says Toner. “Microfluidics gave us an opportunity to more precisely manipulate the blood and see if these cells are there in a useful number.”
A subset of circulating tumor cells in a patient are thought to seed metastases. “In the end, a subpopulation of these cells ends up killing patients,” Toner says. “Finding these cells in patients in real time has tremendous application for monitoring the genotype of the cancer and for early detection.”
The technology gives doctors the ability to monitor cancer over time. “Right now, after a patient is diagnosed with cancer, we don’t usually re-biopsy patients,” says Haber, who is using the devices experimentally to define genetic mutations in lung cancer and match those mutations to therapies. But as a cancer grows and spreads in the body, it changes: “We can’t assume it has the same abnormalities it had at first.”
J&J has partnered with MGH to develop the new chip into a commercial product.
“We see the direction of cancer treatment as the ability to monitor the molecular changes in the disease over time,” says Nicholas Dracopoli, head of oncology biomarkers at Janssen, J&J’s pharmaceutical branch.
The MGH device and some others in development isolate rare cancer cells by discarding all red blood cells and white blood cells, which typically outnumber circulating tumor cells by the billions. Any cancerous cells would then be left in a life-friendly liquid, from which they can be grabbed individually and studied.
Other versions of the technology, including the device that J&J currently sells, capture the cells on a physical surface, usually through a coating of antibodies that recognize proteins on the cell membranes of some, but not all, cancers.
Beyond the potential to improve cancer treatment, devices that can capture circulating tumor cells could help biologists uncover the secrets of cancer’s deadly spread. “The question of how cancer metastasizes and spreads has never really been understood because we didn’t have the tools to study it,” says Haber. “This is the first time that you are looking at cancer cells in transit. They aren’t there long, but they are there.”
Keep Reading
Most Popular
Large language models can do jaw-dropping things. But nobody knows exactly why.
And that's a problem. Figuring it out is one of the biggest scientific puzzles of our time and a crucial step towards controlling more powerful future models.
The problem with plug-in hybrids? Their drivers.
Plug-in hybrids are often sold as a transition to EVs, but new data from Europe shows we’re still underestimating the emissions they produce.
Google DeepMind’s new generative model makes Super Mario–like games from scratch
Genie learns how to control games by watching hours and hours of video. It could help train next-gen robots too.
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.